Case Report | DOI: https://doi.org/CSRR/24/CR/007
Wilms Tumor Metastasis in Frontal Lobe of a Child: Imaging and Surgical Insights of this Very Rare Entity
Abstract
The brain metastasis of Wilms tumor (WT) is a very rare condition identified an average of 0.6% of all patients after this diagnosis. In this case report we sought to present a 9 years old boy who present with a left frontal metastasis of WT after six years of diagnosis and three years of lung metastasis. After total removal of brain tumor and resolution of intracranial hypertension the patient had a good recovery and underwent an adjuvant therapy with radio and chemotherapy. No remission was detected after one year of surgical resection. To the best of our knowledge, this is the first description of surgical aspects of WT brain metastasis and reinforce the good outcome previously reported in the literature.
Introduction
Wilm’s tumor (WT) is a malignant renal tumor and the second most common solid neoplasm affecting one in 10,000 children [1-6]. In spite of the histologically malignance features, the treatment is considered effective in the majority of patients reaching the cure in average of 85% of all cases [7-9]. In addition, is expected that at least 50% of the recurrences will have a prolonged second remission and the most common sites of relapse in WT are the lung, followed by abdomen/flank and liver [10, 11].
Although another renal tumors such as sarcoma and rhabdoid tumor of the kidney have presented the brain as a common site of metastasis, this is a very rare event of WT in which, to date, only two large cooperative groups have published 21 patients with the incidence of 0.6% of the cases [2, 4].
Given that the limited information regarding brain metastasis related to WT, this case report sought to describe a well documented case, giving details of imaging, surgical aspects and histopathological in order to add a meaningful information of this very rare condition.
Case Presentation
The patient has received the diagnosis of WT at the three years old due to a mass detected in the abdomen and underwent a right nephrectomy. After the chemotherapy and radiotherapy, he experienced a remission of disease and with the age of six years old was diagnosed with a metastasis in the inferior lobe of right lung which was removed surgically and received an additional adjuvant treatment with radio and chemotherapy. Afterwards, the patient has an uneventful outcome, presenting high performance on school with a remission of disease.
In the current presentation, a 9 years old boy was attended in the emergency room complaining of headache which was assessed by analogic scale as a level 9 and presenting vomits. Additionally, the boy demonstrated monoparesis of right superior arm with no other deficits on the legs or cranial nerves. Pupils displayed normal reaction to light and no alterations in the conscious were observed. In addition, he presented with dysarthria and no language alterations was observed.
A magnetic resonance imaging (MRI) was performed and revealed a left frontal lobe tumor which exerted mass effect on surroundings (Figure 1 and 2)
A dexamethasone was initiated with partial improve of headache. Therefore a surgical resection was indicated. Further lab analysis was performed with no abnormalities.
Under general anesthesia, the patient was positioned in dorsal decubitus and the head fixed with three pins. A left frontal craniotomy was carried out and the dura opened and pediculated towards superior sagittal sinus. With the aid of intraoperative neurophysiological monitoring the precentral gyrus and motor area was identified in order to minimize injuries. A corticectomy was undertaken and the tumor had a red smooth consistency and tendency to bleed, surrounded by a thin and translucent capsule (Figure 3).
The patient has received the diagnosis of WT at the three years old due to a mass detected in the abdomen and underwent a right nephrectomy. After the chemotherapy and radiotherapy, he experienced a remission of disease and with the age of six years old was diagnosed with a metastasis in the inferior lobe of right lung which was removed surgically and received an additional adjuvant treatment with radio and chemotherapy. Afterwards, the patient has an uneventful outcome, presenting high performance on school with a remission of disease.
In the current presentation, a 9 years old boy was attended in the emergency room complaining of headache which was assessed by analogic scale as a level 9 and presenting vomits. Additionally, the boy demonstrated monoparesis of right superior arm with no other deficits on the legs or cranial nerves. Pupils displayed normal reaction to light and no alterations in the conscious were observed. In addition, he presented with dysarthria and no language alterations was observed.
A magnetic resonance imaging (MRI) was performed and revealed a left frontal lobe tumor which exerted mass effect on surroundings (Figure 1 and 2)
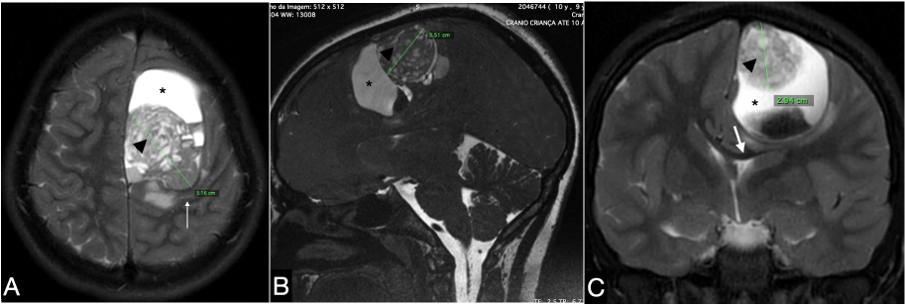
The preoperative brain MRI revealed a large expansive intra-axial lesion in the left frontoparietal lobe presented with an anterior cystic component (*) and a posterior solid component (Arrowhead) measuring 5.16 x 3.51 x 2.84 cm with a heterogeneous aspect. The Axial T2 weighted MRI depicted a compression of precentral gyrus ( Thin write arrow) (A). Sagittal T2 Weighted MRI showed the superficial aspect of the solid portion (B) and the inferior displacement of corpus callosum (Thick write arrow) is observed in the coronal T2 weighted MRI (C).
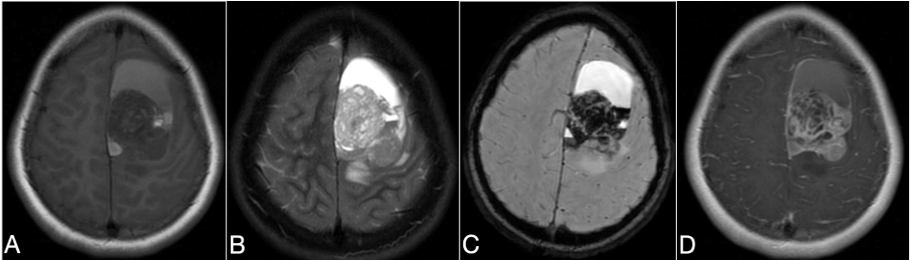
The solid portion of the tumor presented iso/hypo intensity on axial T1 weighted MRI (A), Predominantly hyper in T2 weighted MRI (B), hemorrhage signs were seen on the T2 gradient echo (C). The axial gadolinium enhanced T1 weighted MRI depicted contrast enhancement on the solid lesion(D).
A dexamethasone was initiated with partial improve of headache. Therefore a surgical resection was indicated. Further lab analysis was performed with no abnormalities.
Under general anesthesia, the patient was positioned in dorsal decubitus and the head fixed with three pins. A left frontal craniotomy was carried out and the dura opened and pediculated towards superior sagittal sinus. With the aid of intraoperative neurophysiological monitoring the precentral gyrus and motor area was identified in order to minimize injuries. A corticectomy was undertaken and the tumor had a red smooth consistency and tendency to bleed, surrounded by a thin and translucent capsule (Figure 3).
After the macroscopically total removal of tumor and the complete control of the bleed, the dura was closed with prolen continuous stiches and the bone flap was fixed using absorbable plates and screws. The patient presented an uneventful postoperative period and was discharged from the hospital on the sixth day, experiencing immediate relief of headache and arm monoparesis. As the improvement was achieved, the corticotherapy was discontinued.
The histological profile of tumor was identical of previous surgeries and confirms the WT pattern (Figure 3).
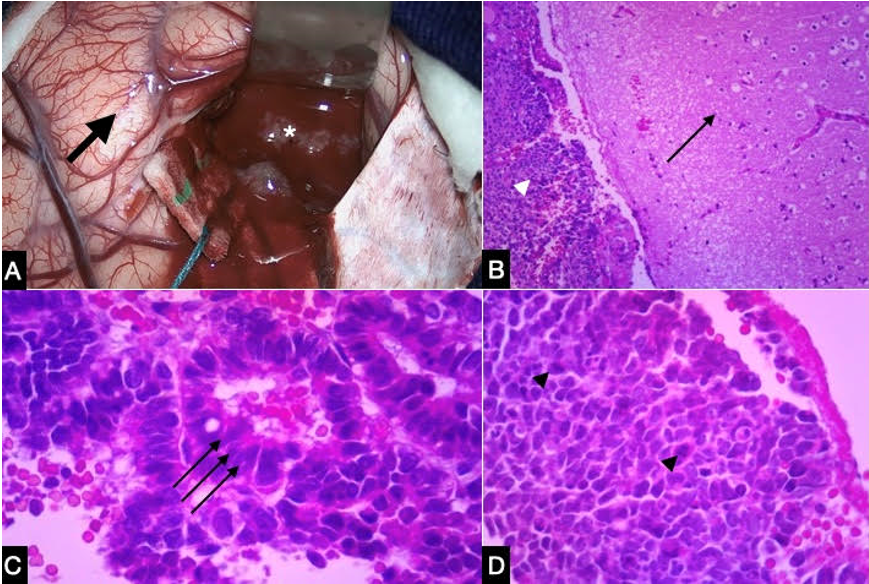
Macroscopically the tumor (*) compressed the left frontal lobe (Thick black arrow) and displayed red color, soft consistency , and high tendency to bleed (A). Microscopically, depicted blastemal component represented by small undifferentiated cells (Write arrowhead) and the normal brain tissue is also showed (Thin black arrow) (B). Epithelial component represented by tubules moderately differentiated (Triple black arrows) is displayed in C. Blastemal component with mitoses( Black arrowheads) in D.
The boy returned of his scholar activities and showed adequate performance. An adjuvant radiotherapy and chemotherapy was performed and the MRI after one year of the surgical removal revealed the complete resection (Figure 4).
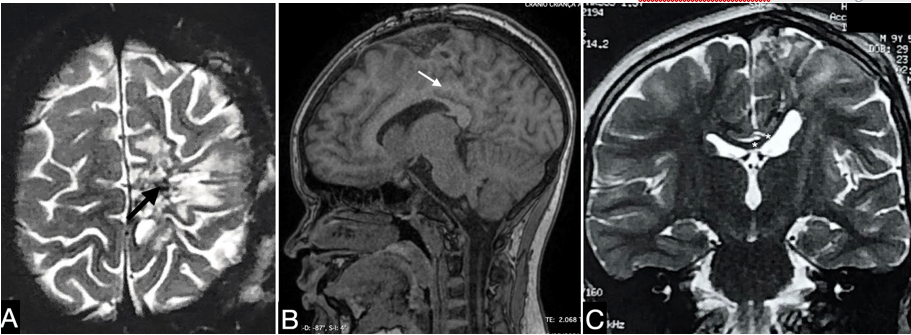
Postoperative image one year after surgery, showing signs of total surgical resection of the lesion. The Axial T2 weighted MRI showed scar formation on the site of tumor resection ( Black arrow)(A). Sagittal T1 weighted MRI depicted recovery of mesial aspect of frontal lobe and the cingulate gyrus ( Write arrow). The recovery of left portion of corpus callosum (*) was observed on the Coronal T2 weighted MRI (C)
Discussion
In this present case report, the brain image displayed a solitary frontal lobe tumor with markedly mass effect, displacing ventricular system and showed heterogeneous aspect with a solid, cystic and hemorrhage signs. Similarly, these features could be seen in others primary supratentorial CNS tumors such as embryonic tumors, pleomorphic xanthoastrocytoma, choroid plexus carcinoma and anaplastic ependymoma, leading this as an important differential diagnosis of this tumor [12-14].
Intraoperatively, the gross surgical removal of this tumor was achieved and technically this was facilitated due to the superficial position in the frontal lobe and its low consistency, which avoids the retraction of the brain. In addition, the intraoperative neurophysiological monitoring contributed to minimize the injury of motor area during tumor remotion. Nonetheless, the tumor displays a hemorrhagic tendency, which could translate in increased risk of morbidity due to hemodynamic instabilization and, several measures such as hemostasis maneuvers and hemostatic sponges was carried out in order to warrant the controle of the blood loss. To our knowledge, this is the first thought surgical description of features of metastatic WT and its complete removal in a single neurosurgical approach. Indeed the anatomical characteristics of this tumor have facilitate its complete removal.
Brain metastase due to WT is a rare event and the evidence is limited to a few studies on literature. So far, two international trials was undertaken and only 21 patients with brain metastasis due to WT were reported with discrepant outcomes were observed. Seven out of 21 children belonged to the United Kingdon Children’s Cancer Study Group (UKCCSG) and three of them remains alive until the publication date [2]. Additionally, the International Society of Pediatric Oncology (SIOP) which followed 3040 patients with WT and reported fatality in all of 14 patients with brain metastasis [15]. Therefore, the current case report could be considered an unusual positive outcome of such patients.
Furthermore, Venkatramani et al [4] conducted a retrospective review of 8609 patients with WT enrolled on the National Wilms Tumor Studies (NWTS) conducted between 1969 and 2002 and found that 47 (0.5%) of patients progressed with intracranial metastasis during the relapse. In addition, 67% of them experienced the brain metastasis after the relapse in another site which the lungs were the more incidence. Moreover, they described a total surgical removal of 11 out of 15 who were underwent a surgical approach and pointed out the best survival profile in those patients with a gross surgical resection and more favorable histology. Similarly, in our case report the patient developed the brain metastasis in the second relapse after three years of resolution of lung relapse and the optimal treatment with gross total resection and adjuvant radiotherapy and chemotherapy were achieved.
Conclusion
Even thought the brain metastasis of WT is rare, the awareness of its imaging characteristics as well as intraoperative pitfalls is paramount especially for the pediatric neurosurgeons and oncologists to diagnose it as soon as possible in order to allow the maximum efficiency of treatment. Therefore, total removal of this type of tumor in combination of adjuvant treatment could mean the satisfatory outcome with quality of life.
References
-
Kebudi R, Ayan I, Gorgun O, Agaoglu FY, Vural S, Darendeliler E: Brain metastasis in pediatric extracranial solid tumors: survey and literature review. J Neurooncol. 2005, 71:43-48.
View at Publisher | View at Google Scholar -
Lowis SP, Foot A, Gerrard MP, Charles A, Imeson J, Middleton H, Coakham H, Bouffet E: Central nervous system metastasis in Wilms' tumor: a review of three consecutive United Kingdom trials. Cancer. 1998, 83:2023-2029.
View at Publisher | View at Google Scholar -
Borni M, Kammoun B, Kolsi F, Abdelhedi A, Boudawara MZ: Isolated central nervous system metastasis in pediatric Wilms' tumor: A case report and review of literature. Urol Case Rep. 2018, 21:78-80.
View at Publisher | View at Google Scholar -
Venkatramani R, Chi YY, Coppes MJ, Malogolowkin M, Kalapurakal JA, Tian J, Dome JS: Outcome of patients with intracranial relapse enrolled on national Wilms Tumor Study Group clinical trials. Pediatr Blood Cancer. 2017, 64.
View at Publisher | View at Google Scholar -
Akakin A, Yilmaz B, Eksi MS, Yapicier O, Kilic T: Relapsed Wilms' tumor with multiple brain metastasis. Korean J Pediatr. 2016, 59:S96-S98.
View at Publisher | View at Google Scholar -
Spreafico F, Bellani FF: Wilms' tumor: past, present and (possibly) future. Expert Rev Anticancer Ther. 2006, 6:249-258.
View at Publisher | View at Google Scholar -
Green DM, Breslow NE, Beckwith JB, Finklestein JZ, Grundy P, Thomas PR, Kim T, Shochat S, Haase G, Ritchey M, Kelalis P, D'Angio GJ: Effect of duration of treatment on treatment outcome and cost of treatment for Wilms' tumor: a report from the National Wilms' Tumor Study Group. J Clin Oncol. 1998, 16:3744-3751.
View at Publisher | View at Google Scholar -
Tournade MF, Com-Nougue C, de Kraker J, Ludwig R, Rey A, Burgers JM, Sandstedt B, Godzinski J, Carli M, Potter R, Zucker JM, International Society of Pediatric Oncology Nephroblastoma T, Study C: Optimal duration of preoperative therapy in unilateral and nonmetastatic Wilms' tumor in children older than 6 months: results of the Ninth International Society of Pediatric Oncology Wilms' Tumor Trial and Study. J Clin Oncol. 2001, 19:488-500.
View at Publisher | View at Google Scholar -
Neville HL, Ritchey ML: Wilms' tumor. Overview of National Wilms' Tumor Study Group results. Urol Clin North Am. 2000, 27:435-442.
View at Publisher | View at Google Scholar -
Groot-Loonen JJ, Pinkerton CR, Morris-Jones PH, Pritchard J: How curable is relapsed Wilms' tumour? The United Kingdom Children's Cancer Study Group. Arch Dis Child. 1990, 65:968-970.
View at Publisher | View at Google Scholar -
Grundy PE, Telzerow PE, Breslow N, Moksness J, Huff V, Paterson MC: Loss of heterozygosity for chromosomes 16q and 1p in Wilms' tumors predicts an adverse outcome. Cancer Res. 1994, 54:2331-2333.
View at Publisher | View at Google Scholar -
Moore W, Mathis D, Gargan L, Bowers DC, Klesse LJ, Margraf L, Koral K: Pleomorphic xanthoastrocytoma of childhood: MR imaging and diffusion MR imaging features. AJNR Am J Neuroradiol. 2014, 35:2192-2196.
View at Publisher | View at Google Scholar -
Berger C, Thiesse P, Lellouch-Tubiana A, Kalifa C, Pierre-Kahn A, Bouffet E: Choroid plexus carcinomas in childhood: clinical features and prognostic factors. Neurosurgery. 1998, 42:470-475.
View at Publisher | View at Google Scholar -
Borja MJ, Plaza MJ, Altman N, Saigal G: Conventional and advanced MRI features of pediatric intracranial tumors: supratentorial tumors. AJR Am J Roentgenol. 2013, 200:W483-503.
View at Publisher | View at Google Scholar -
van den Heuvel-Eibrink MM, Graf N, Pein F, Sandstedt B, van Tinteren H, van der Vaart KE, de Kraker J: Intracranial relapse in Wilms tumor patients. Pediatr Blood Cancer. 2004, 43:737-741.
View at Publisher | View at Google Scholar






