Case Report | DOI: https://doi.org/IJCRI-CR-24-008
Unexpected Giant Sinonasal Osteoma Following Surgery for Chronic Rhinosinusitis with Polyps: A Case Report
Abstract
Osteomas are the most frequently observed benign bone tumors of paranasal sinuses. These slow-growing, benign tumors are often asymptomatic and typically discovered incidentally on radiological exams conducted for unrelated complaints. However, their potential for significant complications arises when they grow to a size or position that impacts adjacent structures. Large osteomas may obstruct sinus drainage, leading to secondary infections such as chronic sinusitis, or extend into the orbit or intracranial space, causing symptoms like proptosis, diplopia, vision loss, headaches, and even cerebrospinal fluid leaks in cases of dural invasion. Intracranial extension, while rare, can lead to serious complications, including meningitis, brain abscess, and mucocele formation. This article presents a 70-year-old male with recurrent chronic rhinosinusitis and nasal polyps, who had undergone functional endoscopic sinus surgery three years prior. At follow-up, the recurrence of nasal polyps was observed alongside a newly developed ethmoidal osteoma. Cases like this underline the importance of regular postoperative imaging, especially in patients with recurrent sinonasal issues, as osteomas can develop post-surgically. Some studies suggest that local factors such as inflammation or surgical trauma may play a role in the growth or initiation of osteomas, though this remains to be fully understood. This case highlights the clinical value of CT and MRI in the identification, differentiation, and management of paranasal sinus osteomas, as well as the importance of vigilance in long-term follow-up for patients with chronic sinonasal conditions.
Introduction:
An ossifying fibroma (OF) is a type of benign fibro-osteoma that rarely involves the sinonasal cavity. About 10% of all cases are found in the maxilla. OF rarely involve the ethmoid sinuses and orbit [1] [2] Recent developments in endoscopic sinus surgery allow the removal of large benign tumors from the nasal cavity and sinuses. Endoscopic resection of OFs is an excellent choice for very experienced surgeons, affording the advantages of direct observation as well as visual enhancement and magnification, thus reducing intra- and post-operative morbidity [3]
Case presentation:
We present the case of a 70 years old male patient, presenting with chronic Rhinosinusitis with polyps, who underwent surgery for chronic rhinosinusitis with polyps three years prior to his admission, with poor adherence to the medical treatment.
The patient presented to the department for the recurrence of a nasal obstruction mainly in the left fossa.
The endoscopic exam showed the recurrence of the nasal polyps.
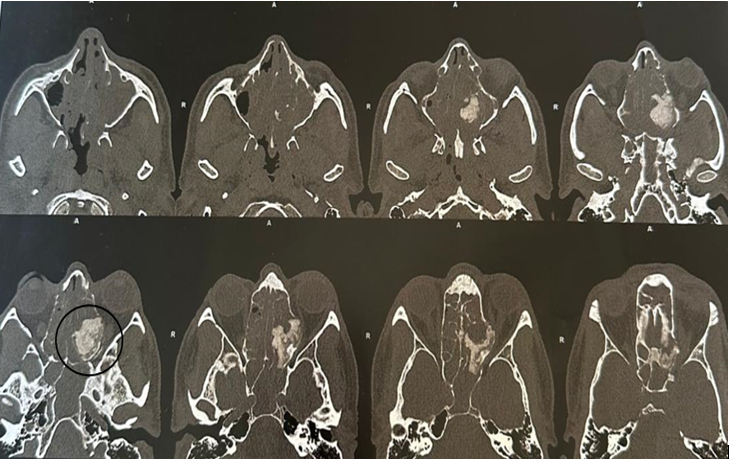
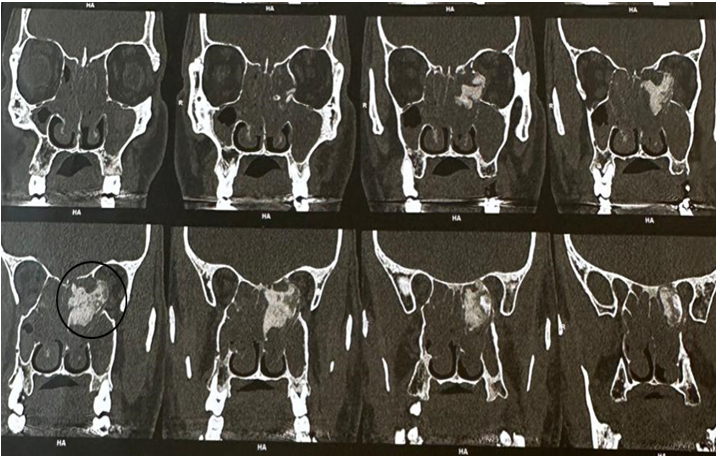
A facial CT-Scan was also performed which revealed a spontaneously enhanced mass in the left posterior ethmoidal cells measuring 35x25 mm. This mass exerts a mass effect on the medial rectus muscle and the medial wall of the left orbit consisting with an ossified fibroma, along with the recurrence of the polyps (Figure 1, 2).
The histopathological finding was consistent with an OF. The tumor mainly consisted of two components: a fibrous stroma, rich in fibroblasts and small vessels surrounded with bony lamellae that were rimmed by osteoblasts and occasionally by osteoclasts.
The ophthalmic examination revealed a grade I exophthalmic without other abnormalities.
The patient underwent surgery and the osteoma was removed (Figure 3) along with the polyps with a good clinical evolution.

Discussion:
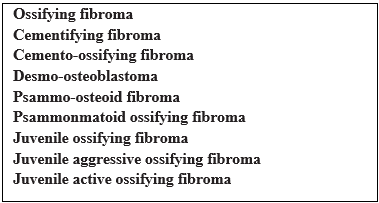
Osteoma is the most common benign tumor of the paranasal sinus, usually occurring in the frontal sinus; however, it is very rare in the nasal cavity. (4) It can be easily differentiated endoscopically from other tumors due to its typical nature. During insertion of the endoscope, most rhinologists usually put the suction tip inside it simultaneously. When the clinician touches the tumor with the suction tip, the osteoma is usually very stiff under palpation. During physical examination, this observation is highly suggestive of nasal osteoma [4] Ossifying fibroma holds a tenuous place in the classification of bony lesions. It was first mentioned by Menzel in 1872, who considered it to be a form of osteoma [5]. OF is classified as a benign fibro-osseous lesion, a term that is synonymous with a variety of lesions reported in available literature (Table I).
The origin of OF is debated with a predominant theory claiming the tumor originates from periodontal roots because of their capacity to produce cementum and osteoid tissue [5] OF typically presents in the mandible (75%) and thus is usually reported and treated by oral surgeons. Other reported locations of OF are maxilla, frontal bone, sphenoid bone, ethmoid bone, temporal bone, orbit, anterior cranial fossa and auricula. [2]
The otolaryngologist’s concern lies with the extramandibular presentation because OF is believed to behave more aggressively than its mandibular counterpart and requires complete surgical resection [3,6]. Presenting symptoms of OF depend on the location of the tumor and range from nasal obstruction to disfiguration. Individual patients may present with ophthalmologic symptoms, such as proptosis and diplopia. Intracranial extension of OF fibroma itself or associated mucoceles may give rise to neurological symptoms. [1,4]
Patients with OF range from newborns to those in their eighth decade of life, with more aggressive behavior at an earlier age. The highest incidence of OF is reported between the ages of 20 to 40 years with a female predilection [7–9]
It is usually discovered incidentally but it can be locally aggressive. The lesion is best imaged by CT scan, with MRI serving for surgical planning or evaluation of complications. Imaging features vary with the amount of fibrous and bony tissue within the lesion, being typical in early stages the presence of a thick peripheral rim of bone surrounding a fibrous soft-tissue center, occurring progressive filling of this center with mature bone in later stages [10]
In a study realized by Nassrallah et al [11], chronic rhinosinusitis with nasal polyps (CRSwNP) was associated with hamartoma tumors 40% and 60% association with Schneiderian papilloma, chronic polyposis sinusitis associated with tumor pathology – 33% with osteoma, 34% with intestinal type adenocarcinoma, 33% with ameloblastoma. The association of tumors of different types, benign or malignant with polyposis inflammatory phenomena was highlighted in this study, and corresponds to international multicenter studies, which show the high risk that nasal polyposis can play in triggering nasal and nasal-sinus malignancies [12,13].
Although malignant transformation in OF has not been reported, surgery is the treatment of choice. Complete resection of extramandibular ossifying fibroma (OF) is curative, with the surgical approach tailored to the tumor’s location and extent. Various open techniques have been reported for this, including the Caldwell-Luc procedure and curettage with peripheral ostectomy for tumors in the maxillary sinus floor; lateral rhinotomy with medial maxillectomy for tumors on the medial wall of the maxillary sinus; and external ethmoidectomy for recurrent ethmoid tumors. Additionally, transcranial/subcranial and subfrontal approaches are also utilized for specific cases]. Advances in endonasal endoscopic sinus surgery have enabled the resection of large benign sinonasal and cephalonasal tumors. The endonasal endoscopic approach offers advantages such as direct visualization, enhanced visibility, and magnification, leading to reduced intraoperative trauma and postoperative morbidity.
Conclusion:
Ossifying fibroma is a fibro-osseous lesion that occurs mainly on the mandibular and maxillary bones and rarely on paranasal sinuses. The association of this tumor with a chronic rhinosinusitis with polyps is rare. It is often revealed with the CT scan imaging and may present with different signs regarding its location. In the paranasal sinuses, the complete resection is curative, and must preserve the noble regions around the tumor. The endoscopic approach allows good results and can guarantee the complete resection. It is always necessary to confirm the diagnosis by the histopathological examination, although malignant transformation in OF has not been reported.
References
-
Godt A, Gülicher D, Kalwitzki M, Kröber SM. Dislocation of an upper third molar by an ossifying fibroma--case report. J Craniomaxillofac Surg. sept 2008;36(6):360‑364.
View at Publisher | View at Google Scholar -
Jurlina M, Skitarelić N, Passali D, Passali FM, Mladina R. Endonasal endoscopic resection of ossifying fibroma involving the ethmoid sinus, orbit and anterior skull base: case report and literature review. Acta Otorhinolaryngol Ital. avr 2016;36(2):144‑148.
View at Publisher | View at Google Scholar -
Wang Y, Cao Z, Gu Z. Endoscopic Resection of a Massive Ossifying Fibroma in the Sinonasal Cavity. J Craniofac Surg. 1 août 2021;32(5):1800‑1802.
View at Publisher | View at Google Scholar -
Kim JS, Noh SJ, Ryu SH. Osteoma with actinomycosis in a nasal cavity: A case report. Medicine (Baltimore). déc 2017;96(51):e9376.
View at Publisher | View at Google Scholar -
Brademann G, Werner JA, Jänig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. The Journal of Laryngology & Otology. févr 1997;111(2):152‑155.
View at Publisher | View at Google Scholar -
London SD, Schlosser RJ, Gross CW. Endoscopic management of benign sinonasal tumors: a decade of experience. Am J Rhinol. 2002;16(4):221‑227.
View at Publisher | View at Google Scholar -
Al-Mazrou KA, Mansoor A, Payne M, Richardson MA. Ossifying fibromyxoid tumor of the ethmoid sinus in a newborn: report of a case and literature review. International Journal of Pediatric Otorhinolaryngology. 1 févr 2004;68(2):225‑230.
View at Publisher | View at Google Scholar -
Johnson LC, Yousefi M, Vinh TN, Heffner DK, Hyams VJ, Hartman KS. Juvenile active ossifying fibroma. Its nature, dynamics and origin. Acta Otolaryngol Suppl. 1991;488:1‑40.
View at Publisher | View at Google Scholar -
Bohn OL, Kalmar JR, Allen CM, Kirsch C, Williams D, Leon ME. Trabecular and Psammomatoid Juvenile Ossifying Fibroma of the Skull Base Mimicking Psammomatoid Meningioma. Head and Neck Pathol. 1 mars 2011;5(1):71‑75.
View at Publisher | View at Google Scholar -
Salina ACI, Souza PMM de, Gadelha CM da C, Aguiar LB, Castro JDV de, Barreto ARF. Ossifying fibroma: an uncommon differential diagnosis for T2-hypointense sinonasal masses. Radiol Case Rep. juin 2017;12(2):313‑317.
View at Publisher | View at Google Scholar -
Nassrallah S, Neagoş CM, Mocan SL, Neagoş A. Evaluation of the incidence of inflammatory and tumor pathology of nose and nasal sinus region. Rom J Morphol Embryol. 2020;61(4):1295‑1300.
View at Publisher | View at Google Scholar -
Eschenbacher WH, Borish L. Nasal polyposis and future risk of sinonasal malignancy. Journal of Allergy and Clinical Immunology. 1 oct 2019;144(4):933‑934.
View at Publisher | View at Google Scholar -
Arslan F, Tasdemir S, Durmaz A, Tosun F. The effect of nasal polyposis related nasal obstruction on cognitive functions. Cogn Neurodyn. 1 août 2018;12(4):385‑390.
View at Publisher | View at Google Scholar






