Research Article | DOI: https://doi.org/10.5281/zenodo.18654711
Therapeutic Hypothermia (TH) for Neonatal Hypoxic Ischemic Encephalopathy (HIE) in Low- and Middle-Income Countries (LMIC’s): Efficacy and Safety of Ice Gel Packs as a Low-Cost Tool
Abstract
Aim: To assess the efficacy and safety of ice gel packs as a manual method of therapeutic hypothermia in Term and Near-Term newborn infants admitted with Moderate and Severe Hypoxic Ischemic Encephalopathy.
Background: TH is a standard prophylactic neuroprotective therapy for Neonatal HIE. TH can be provided either by servo-controlled method (which is expensive) or by manually controlled method (which is inexpensive). This manuscript shares our experience of use of Ice Gel packs as a manual method of TH. The findings have implications for LMIC’s.
Material and Methods: A retrospective cross sectional observational study was carried out in tertiary care NICU of Dr. Sulaiman Al Habib Hospital Al Qassim KSA. Demographic and clinical data was collected, on pre-approved Performa, using patient electronic health records. The data items included hourly temperature record, neurological examination, relevant labs and MRI results. The data was tabulated and analyzed by SPSS version 23 (IBM Corp, Amonk, NY, USA) software.
Results: 23 neonates, born between 2020 and 2023, and admitted with a diagnosis of moderate to severe HIE and provided cooling therapy using Ice gel packs, were included in the study. In all babies, core body temperature was effectively controlled between 330 C and 340 C for 72 hours followed by a very smooth slow rewarming to normal temperature over a period of eight hours. There was no mortality and no significant long term morbidity. The neurodevelopmental examination was normal on discharge and on follow up after one month.
Conclusion: Ice gel packs are a safe and effective low-cost method of achieving target therapeutic hypothermia in newborn babies with Hypoxic Ischemic Encephalopathy. The finding has significant clinical and financial implications for newborn care in LMIC.
Introduction
Despite many interventions, HIE remains an important cause of neonatal mortality and morbidity. In 2021, the global incidence of HIE was estimated at 8.2/1000 live births, contributing to over 600,000 deaths each year [1,2]. Overall incidence of HIE is around 1 per 1000 live births in developed countries and it is around 10 times higher in developing countries [3,4]. The best predictor of mortality and morbidity is the severity of neonatal encephalopathy secondary to Perinatal Asphyxia [5]. With increasing severity of encephalopathy, the incidence of mortality and disability becomes higher. About one third of new-borns with moderate HIE will have some kind of neurological disability. 15% to 20% of infants with HIE die in the neonatal period and 25-30% of survivors develop long-term neurodisability [6].
Therapeutic Hypothermia (TH) is a safe, effective and established neuroprotective intervention for reducing mortality and morbidity in term and near-term new-born infants with moderate and severe HIE [7]. TH can be provided by selective head cooling or total body cooling. Total body cooling is a preferred method due to proven benefits in improving the outcome and reducing neurological disability [8].
Various devices are used for total body cooling. These include servo-controlled cooling machines (which are expensive) and manual cooling methods (which are inexpensive). Cooling blankets, ice gel packs, water bottles, phase changing materials and electric fans have been used for manual cooling [9]. The Servo-controlled methods can be superior in thermoregulation but according to Buchiboyina A et al, [10] there is no difference in neurodevelopmental outcome at 18 months of age. Manual cooling methods are very useful in resource constrained setting of LMIC which bear the burden of 98% of cases of Perinatal Asphyxia worldwide [11]. In this manuscript we share our experience of use of ice gel packs for providing TH in term and near-term infants with Hypoxic Ischemic Encephalopathy.
Material and Methods:
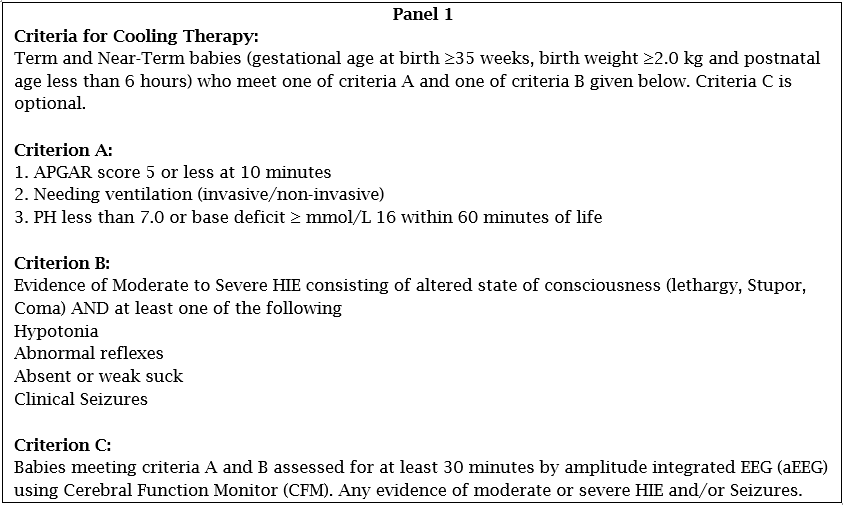
This is a retrospective cross-sectional cohort study conducted in newborn infants admitted to NICU of Dr Sulaiman Al Habib Hospital, Qassim from Jan 2020 to Dec 2023. The study and its data collection form were approved by the institutional review board (IRB). The inclusion criteria for the study included all babies who completed 72 hours of cooling followed by eight hours of gradual rewarming. The exclusion criteria included those babies who could not complete cooling & rewarming as per standard protocol. The criteria for cooling are given in Panel 1.
Cooling was started as soon as possible within first 6 hours after establishment of diagnosis of HIE. Cooling was continued for 72 hours during which rectal temperature was maintained between 330C to 340C using ice gel packs. Rectal temperature probe was used for continuous electronic monitoring of core body temperature. Hourly temperature records were maintained till complete rewarming back to normal body temperature (36.80C) was achieved. Rewarming was done slowly at a rate not more than 0.50C per hour over a period of eight hours. All babies received 1:1 nursing care during the acute phase of their illness.
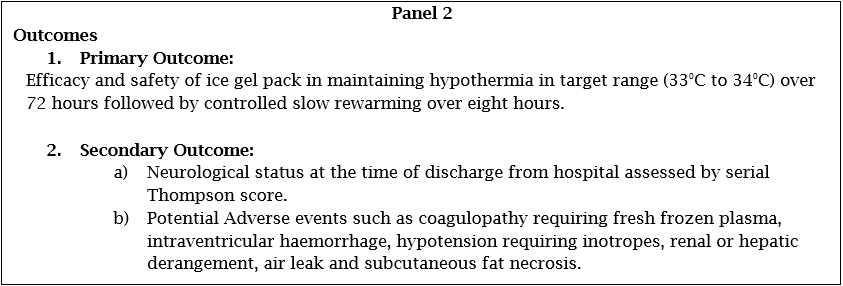
Demographic and clinical data including hourly rectal temperature records, lab investigations, neurological examination findings, ultrasound and MRI reports were retrieved from patient’s electronic medical records. Hourly rectal temperature records were plotted in graphic form for the trends in maintenance of TH during 72 hours of cooling and eight hours of rewarming within the protocol limits. Data was also analysed for associated risk factors of HIE, outcomes at discharge and on first follow up visit at one month. Post cooling MRI scans were used as a surrogate to predict outcomes. [11,12] MRI was performed on D 5 of life under General anaesthesia to minimize motion artifacts and was reported by neuroradiologist. The measured outcomes are given in Panel 2.
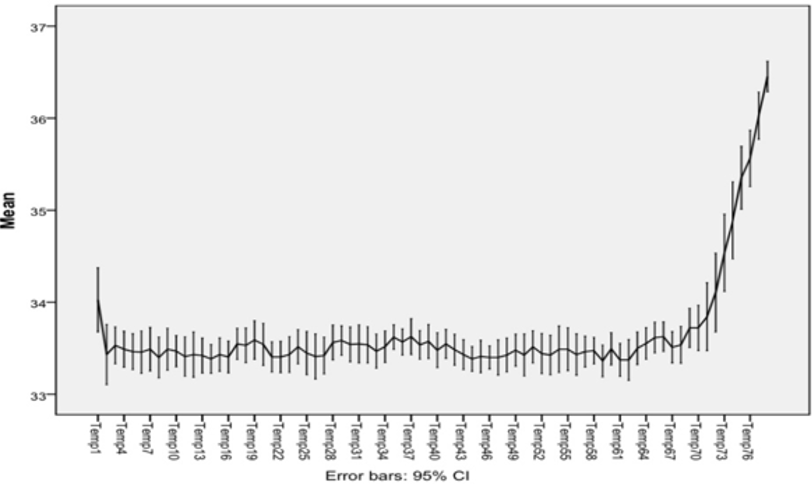
Data was entered into Microsoft Excel sheet and then analysed using SPSS version 23 (IBM Corp, Amonk, NY, USA) software. Quantitative variable like gestational age and weight were tabulated as mean and standard deviation. Qualitative variables like gender, presence or absence of coagulopathy were tabulated as percentages. Hourly temperature control over 72 hours of cooling followed by eight hours of rewarming was plotted as line graph [15]. (Figure.1)
Results:
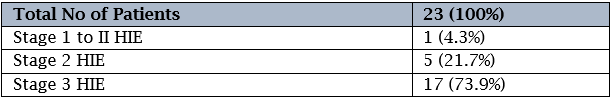
During study period 23 neonates were admitted to NICU with HIE and given cooling therapy. Initial scoring was done using Modified Sarnat & Sarnat score. Accordingly, babies were classified as having Stage I, II or III HIE. Five patients had Stage II HIE, 17 had stage III HIE and one had stage I to II HIE (Table 1).
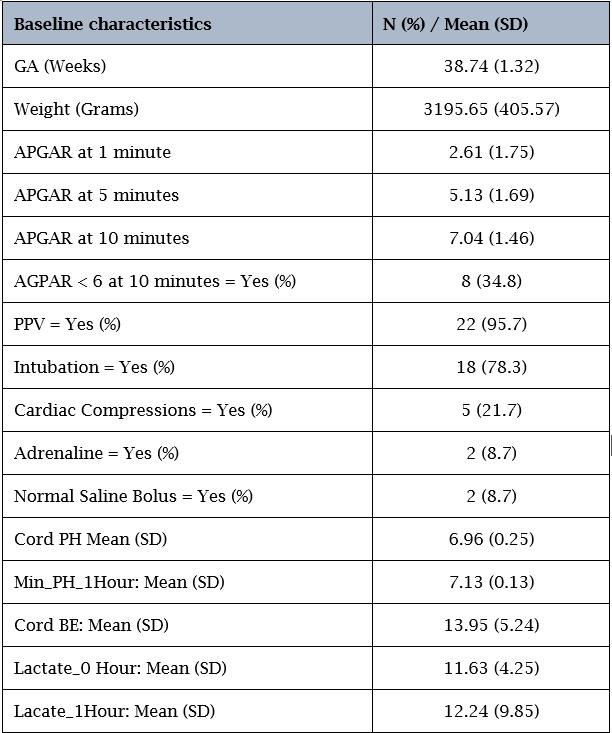
Condition of babies at birth and resuscitation details are given in Table 2. The mean APGAR score at birth was 2.61 and at 10 minutes of life 34% of babies had APGAR score less than 6. All babies required respiratory support at birth and 78% of them were intubated requiring mechanical ventilation. Only 5 babies needed chest compression of which two received adrenaline at time of cardiopulmonary resuscitation.
Mean temperature value was calculated for each 4 hours with standard deviation and plotted on the chart shown in Figure 1. All mean temperature values occurred between 33°C and 34°C
During 72 hours of cooling, 17 patients developed coagulopathy requiring treatment with Vitamin K and Fresh Frozen Plasma (FFP). The coagulopathy was transient and resolved within the cooling period. Renal function derangement was observed in 26% of patients while 47 % had elevated liver enzyme. However, all derangements resolved without any intervention, and none progressed to end stage renal or liver disease.
Of the 23 patients enrolled, MRI was performed in 22; one patient’s family declined the procedure. Six patients had normal MRI, fifteen showed moderate hypoxic-ischemic changes and one had severe hypoxic ischemic changes. Unilateral grade one intracranial haemorrhage was detected in three patients and unilateral grade two intracranial haemorrhage was detected in one patient on day one of life by cranial ultrasonography and later confirmed by MRI on day five of life. Two patients developed subcutaneous fat necrosis; one on the back and one on the hand, both of which resolved with conservative management. No mortality was reported. One neonate with meconium aspiration syndrome required prolonged NICU admission of more than one month with extended respiratory support. Seventeen patients developed seizures and were treated with antiepileptic drugs; fifteen of them were discharged home on antiepileptics therapy (Table: 3).
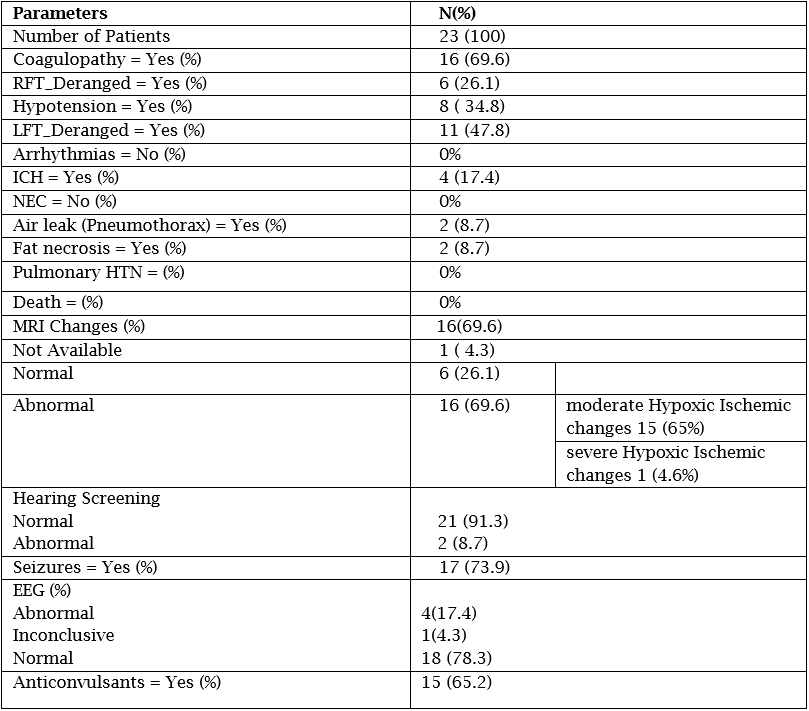
Abbreviations: GA: Gestational Age, RFT: Renal Function Test, LFT: Liver Function Test, ICH: Intracranial Haemorrhage, NEC: Necrotising Enterocolitis, HTN: Hypertension, EEG: Electroencephalograph
Outcome At Discharge:
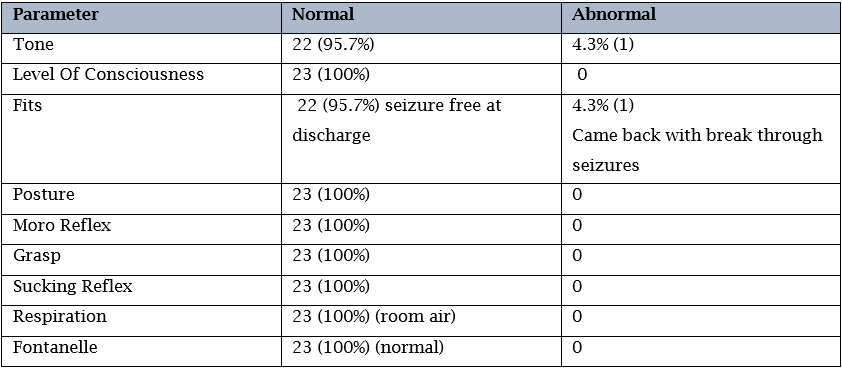
All 23 babies were discharged home alive. Neurological examination at discharge was done using Thompson score (Table 4). One baby had abnormal examination at discharge and one baby was readmitted due to breakthrough seizures. Twenty-one babies had normal examination.
Discussion:
Hypoxic Ischemic Encephalopathy (HIE) is an important cause of Neonatal Mortality and Morbidity worldwide. Globally the incidence of HIE is estimated at 8.3 per1000 live birth with substantial disparities between high income and low-and middle-income countries (LMIC). In high income countries like USA, the estimated incidence is 1 to 3 per 1000 live births while in LMIC countries it is recorded from 4 to 24 per 1000 live births [1-3]. Nearly 99 % of HIE related mortality occurs in LMIC due to limited resources and inadequate health care services [4].
The most effective and safe neuroprotective intervention for management of HIE, which is known to improve neurological outcome, is whole body cooling [5-6]. The concept of hypothermia in medicine is ancient. There are multiple animal studies which proved benefit of hypothermia in reduction of extent of brain damage due to ischemia [11]. Multiple clinical trials have proved therapeutic benefit of Therapeutic Hypothermia (TH) in limiting extent of brain damage if initiated within the first 6 hours of life and continued for 72 hours [7-13]. Eleven randomized controlled trials were included in Cochrane metanalysis 2013, according to which cooling reduces neonatal mortality and morbidity without any additional increase in risk of long-term disabilities in survivors [14]. Therapeutic Hypothermia (TH) is now an established intervention worldwide for term and near-term infants with moderate to severe Perinatal Hypoxic Ischemic Encephalopathy. However, the implementation of TH in LMIC’s remains a very big challenge due to cost effectivity and affordability [15,16].
Attributing to the high burden of birth asphyxia, limited resources and inadequate health systems in LMIC’s, there is need for a cost-effective intervention to reduce neonatal mortality and morbidity due to HIE. Servo controlled cooling machines are very expensive and unaffordable by NICU’s in LMIC’s. Our study has confirmed that inducing and maintaining TH by using Ice gel packs is a very safe, effective and affordable alternative to servo-controlled machines. Other similar studies have also confirmed the same [16]. The ICE trial used ice gel packs for TH in developed countries [17]. The clinical trials, both in high income and LMIC, have confirmed the safety and efficacy of ice gel packs under strict protocol and appropriate training [15,17].
Bharadwaj SK and Bhat BV [16] compared the use of Ice gel packs and servo-controlled machine for management of neonates with HIE. Their study confirmed that TH using ice-gel packs can reduce the risk of neonatal death and neurodevelopmental delay at 6 months of age. Ice gel pack group had better outcomes as compared to servo control group and difference was statistically significant. No difference was noted in terms of complications or any adverse events.
Mascarenhas et al [18] studied short- and long-term outcome and complications of therapeutic hypothermia. Reported adverse events included shock (50.3%), clinically significant bleeding (16%), acute kidney injury (6.7%), culture-positive sepsis (11.6%), persistent pulmonary hypertension (9%), bradycardia (9%), food intolerance (14.9%) and premature termination of TH (7.1%). [18] In our study, 69% patients had coagulation abnormalities 26% had renal impairment and 47% had hepatic derangements. 34% patients suffered from hypotension requiring ionotropic support. Two patients developed subcutaneous fat necrosis which resolved with conservative management. The survival in our cohort was 100 % and 95.7% had normal neurological examination on discharge. Prakash et al [19], in a recent meta-analysis on TH for HIE in LMIC, did not find any difference in mortality in cooled and non-cooled infants. However, the cooled group exhibited significantly lower rates of neurodevelopmental disability at or beyond 6 months (RR 0.78, 95% CI 0.66–0.92, I2 = 85%) [19] .
Trials of neuroprotective strategies other than TH are underway [1]. lt is crucial that new interventions should not only be feasible for use in LMIC’s, but also that LMIC’s should conduct research to evaluate the cost-effectiveness of new interventions in their settings [20]. Research should also be done on the safety, efficacy and feasibility of neuroprotective pharmacologic agents, either alone or in combination with TH, in the context of LMIC’s. The safety of combination of TH and MgSO3 for moderate to severe HIE in term and near-term infants has already been reported from LMIC [21]. Our study has confirmed safety and efficacy of ice gel packs in achieving target temperature for TH. These developments have positive implications for managing new-born infants with HIE in resource restricted LMIC’s [22].
Conflict of Interest:
None
Limitation of our Study:
Due to small sample size results are limited and no correlation can be established between severity of HIE and neurological outcome. Due to absence of long term follow up it is difficult to ascertain the degree of any long-term neurodevelopmental impairment.
Conclusion:
Ice-gel packs can be used as a safe and effective alternative to servocontrolled devices for whole body therapeutic hypothermia in term and near term neonates with hypoxic ischemic encephalopathy (HIE), when applied with careful temperature monitoring and good nursing care.
References
-
Altirkawi K. Therapeutic Hypothermia in neonatal encephalopathy: current challenges and future prospects. Academia Medicine 2025;2. (https://doi.org/10.20935/AcadMed7908)
View at Publisher | View at Google Scholar -
Spain JE, Tuuli MG, Macones GA, Roehl KA, Odibo AO, Cahill AG. Risk factors for serious morbidity in term non anomalous neonates. Am J Obstet Gynecol [Internet]. 2015;212(6):799.e1-799.e7. (Available from: http://dx.doi.org/10.1016/j.ajog.2015.01.028)
View at Publisher | View at Google Scholar -
Acun C, Karnati S, Padiyar S, Puthuraya S, Aly H, Mohamed M. Trends of neonatal hypoxic-ischemic encephalopathy prevalence and associated risk factors in the United States, 2010 to 2018. Am J Obstet Gynecol2022; 227(5):751.e1-751.e10. (Available from: http://dx.doi.org/10.1016/j.ajog.2022.06.002)
View at Publisher | View at Google Scholar -
Gannon H, Chimhini G, Cortina-Borja M, Chiyaka T, Mangiza M, Fitzgerald F, Heys M, Neal SR, Chimhuya S. Risk factors of mortality in neonates with neonatal encephalopathy in a tertiary newborn care unit in Zimbabwe over a 12-month period. PLOS Glob Public Health. 2022 Dec 20;2(12):e0000911. doi: 10.1371/journal.pgph.0000911. PMID: 36962805; PMCID: PMC10021203.
View at Publisher | View at Google Scholar -
Mosalli R. Whole body cooling for infants with hypoxic-ischemic encephalopathy. J Clin Neonatol. 2012;1(2):101. Available from: http://dx.doi.org/10.4103/2249-4847.96777
View at Publisher | View at Google Scholar -
Itoo BA, Al-Hawsawi ZM, Khan AH. Hypoxic ischemic encephalopathy. Incidence and risk factors in North Western Saudi Arabia. Neurosciences (Riyadh). 2003;8(2):113–9.
View at Publisher | View at Google Scholar -
Lemyre B, Chau V. Canadian Paediatric Society Fetus and Newborn Committee. Paediatr Child Health. 2018;23(4):285–91.
View at Publisher | View at Google Scholar -
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic–ischemic encephalopathy. N Engl J Med. 2005;353(15):1574–84. Available from: http://dx.doi.org/10.1056/nejmcps050929
View at Publisher | View at Google Scholar -
Shah M, Sakr M, Balasundaram P. Neonatal Therapeutic Hypothermia. [Updated 2025 Sep 14]. In: Stat Pearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567714/
View at Publisher | View at Google Scholar -
Buchiboyina A, Ma E, Yip A, Wagh D, Tan J, McMichael J, et al. Servo controlled versus manual cooling methods in neonates with hypoxic ischemic encephalopathy. Early Hum Dev. 2017;112:35–41. Available from: http://dx.doi.org/10.1016/j.earlhumdev.2017.06.011
View at Publisher | View at Google Scholar -
Prashantha YN, Suman Rao PN, Nesargi S, Chandrakala BS, Balla KC, Shashidhar A. Therapeutic hypothermia for moderate and severe hypoxic ischaemic encephalopathy in newborns using low-cost devices – ice packs and phase changing material. Paediatr Int Child Health. 2019;39(4):234–9. Available from: http://dx.doi.org/10.1080/20469047.2018.1500805
View at Publisher | View at Google Scholar -
Rollins N, Booth T, Morriss MC, Sanchez P, Heyne R, Chalak L. Predictive value of neonatal MRI showing no or minor degrees of brain injury after hypothermia. Pediatr Neurol. 2014 May;50(5):447-51. doi: 10.1016/j.pediatrneurol.2014.01.013. Epub 2014 Jan 7. PMID: 24656462; PMCID: PMC4006931
View at Publisher | View at Google Scholar -
Roka A, Azzopardi D. Therapeutic hypothermia for neonatal hypoxic ischaemic encephalopathy. Early Hum Dev. 2010;86(6):361–7. Available from: http://dx.doi.org/10.1016/j.earlhumdev.2010.05.013
View at Publisher | View at Google Scholar -
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Libr. 2013; Available from: http://dx.doi.org/10.1002/14651858.cd003311.pub3
View at Publisher | View at Google Scholar -
Ballot DE, Ramdin TD, Bandini RM, Nakwa F, Velaphi S, Coetzee M, et al. Therapeutic hypothermia for neonatal hypoxic ischaemic encephalopathy should not be discontinued in low- and middle-income countries. S Afr Med J ;111(12):1168–9. Available from: http://dx.doi.org/10.7196/SAMJ.2021.v111i12.16180
View at Publisher | View at Google Scholar -
Bharadwaj SK, Bhat BV. Therapeutic hypothermia using gel packs for term neonates with hypoxic ischaemic encephalopathy in resource-limited settings: a randomized controlled trial. J Trop Pediatr. 2012;58(5):382–8. Available from: http://dx.doi.org/10.1093/tropej/fms005
View at Publisher | View at Google Scholar -
Jacobs SE. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: A randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(8):692. Available from: http://dx.doi.org/10.1001/archpediatrics.2011.43
View at Publisher | View at Google Scholar -
Mascarenhas D, Goyal M, Nanavati R, Kirthana SB, Subhadarsini S. Short-term outcome and complications of therapeutic hypothermia in neonates with moderate-to-severe hypoxic ischaemic encephalopathy: a single-centre retrospective observational study in a hospital in Mumbai, India. Paediatr Int Child Health. 2022;42(3–4):117–26. Available from: http://dx.doi.org/10.1080/20469047.2023.2171762
View at Publisher | View at Google Scholar -
Prakash R, Reyes-Garcıa DV et al. J Trop Pediatr Therapeutic hypothermia for neonates with hypoxic-ischaemic encephalopathy in low- and lower-middle-income countries: a systematic review and meta-analysis., 2024, 70(5),1-18.
View at Publisher | View at Google Scholar -
Tagin M, Abdel-Hady H, Rahman S et al. Neuroprotection for Perinatal Hypoxic Ischemic Encephalopathy in Low- and Middle-Income Countries. J Peds 2015. 167 (1);27-28
View at Publisher | View at Google Scholar -
Rahman SU, Canpolat FE, Oncel MY, Evli A, Dilmen U, Parappil H, et al. Multicenter randomized controlled trial of therapeutic hypothermia plus magnesium sulfate versus therapeutic hypothermia plus placebo in the management of term and near-term infants with hypoxic ischemic encephalopathy (The Mag Cool study): A pilot study. J Clin Neonatol 2015;4:158-63.
View at Publisher | View at Google Scholar -
Rahman SU. Whole Body Hypothermia, Using Low-Cost Technique, is Safe and Effective in Term and Near-Term Babies with Moderate and Severe Hypoxic Ischemic Encephalopathy. JCN 1(1):p 15-17, Jan–Mar 2012. | DOI: 10.4103/JCNEO_20120101_15
View at Publisher | View at Google Scholar






