Research Article | DOI: https://doi.org/WHRWB/RA/003
The Hemodynamic Instability at the Pediatric Hospital
Abstract
Introduction: Hemodynamic instability refers to a compromised ability to move the blood around, which if left untreated can lead to inadequate tissue per- fusion, organ failure, and possibly death. It may also be defined as one or more out-of-range vital sign measurements, such as systolic blood pressure (SBP) < 90mmHg or ≥160 mmHg, Mean Arterial Pressure (MAP) less than 65, tachycardia >100beats per min or bradycardia<50 beats per min or shock index (OSI)>0.9 beats per mmHg. In the obstetric patient, hemodynamic compromise may manifest as hypotension or hypertension, as the result of conditions such as obstetric hemorrhage and sepsis causing hypotension, but also the hypertensive disorders of pregnancy.
Objective: We aimed to study the frequency, etiology, management and prognosis of obstetric hemodynamic instability at the Yaoundé Gyneco-Obstetric and Pediatric Hospital.
Methodology: We conducted a cross sectional analytic study of all pregnant and post-partum patients who were diagnosed with hemodynamic instability irrespective of the cause at the Yaoundé Gyneco-Obstetric and Pediatric Hospital between 1st April 2022 and 31st August 2022. We included all pregnant and post-partum patients who were diagnosed with one or more of the following: SBP < 90mmHg or ≥160 mmHg, MAP<65, heart rate>100bpm and OSI>1 and patients who gave their consent. We didn’t include patients without consent, nor those with non-obstetric causes of hemodynamic instability. We used the software SPSS version 1.0.0.1406 for statistical analysis.
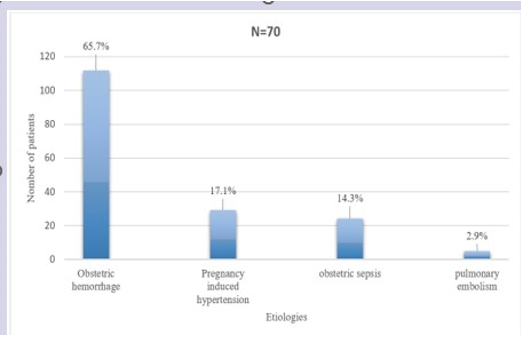
Results: During the study, a total of 1298 deliveries and 70 obstetric hemodynamically unstable patients were assessed, giving us a frequency of 5.4%. Patients were aged between 20 to 30 years (60%) with a mean maternal age of 27.3 ±5.2 years. They were mostly students (52.9%), had a secondary educational level (55.7%) and were single (75.7%). They were mostly primiparous (35.7%) and pauciparous (44.3%). Most of our patients were unbooked (38.6%) or poorly booked (44.3%) for antenatal care. They were mostly referred from health centres (75.7%) without an intravenous line (60.9%). Obstetric hemorrhage was the most frequent cause of obstetric hemodynamic instability with 65.7%, followed by pregnancy induced hypertension in 17.1%, obstetric sepsis (14.3%) and pulmonary embolism (2.9%). In our study, 74.3% had a favourable outcome and (25.7%) were unfavourable amongst which maternal death accounted for 20% and 5.7% had acute kidney injury. Caesarean section (40.3%) and laparotomy (38.2%) were the most frequent surgical treatment to manage the causes of obstetric hemodynamic instability. All our patients were placed on antibiotics, Oxygen supplementation 62.9% and blood transfusion 77.1% Which were also required in majority of the patients. The probable factors of poor maternal outcome were unmarried patients (OR=4.6; IC= 0.41-103.81; p-value =0.0088), a delay of more than 6hrs between the onset of symptoms and consultations (OR=2.6; C.I (0.5, 18.8); p-value=0.046), a delay of more than 1h between con- sultation and management (OR=3.3; C.I (0.98, 28.9); p- value=0.001), being consulted by a midwife (OR=8.6; C.I (2.2, 43.2); p-value=0.004) and an obstetric shock index of 0.98 and above (OR=4.04; C.I (0.98, 88.7); p-value=0.054).
Conclusion: obstetric hemodynamic instability is frequent in our context and under diagnosed. The consequences are lethal especially when there is delay in the management.
Introduction:
This was a cross sectional analytic study of all pregnant and post-partum patients who were diagnosed with hemodynamic instability irrespective of the cause at the YGOPH between 1st April 2022 and 31st August 2022.
After the validation of our protocol and obtention of an ethical clearance from competent authorities. When the permission was granted, patients were recruited from external consultation, intensive care unit and emergencyward and a consent form was submittedfor approval to each patient. We identified all pregnant and post-partum patients who were diagnosed with one or more of the following: SBP < 90mmHg>100bpm and OSI>1. The patients were recruited from external consultation, labor room, hospitalward, intensive care unit and emergencyward. A consent form was submittedfor approval to each patient or their caretaker for those patients who wereunstable or unconscious. We retrieved other information from the patient’s medicalfile and antenatal consultation book. We did not include patients who refused to give their consent.
Results and Discussion:
Study limitation
In this survey, we sought to study obstetric hemodynamic instability at the Yaoundé Gynaeco-Obstetrics and Pediatric Hospital (YGOPH). This was a cross sectional analytic study of all pregnant and post-partum patients who were diagnosed with hemodynamic instability irrespective of the cause at the YGOPH between 1st April 2022 and 31st August 2022. The main limitation was the fact that, being a single centered study, our results cannot be extrapolated to a larger and diverse base of obstetric patients. Multi-Centre Cameroon studies on obstetric hemodynamic instability may be helpful.
Frequency
During the study, a total of 1298 deliveries and 70 obstetric hemodynamically unstable patients were diagnosed between 1st April 2022 and 31st August 2022, giving us an incidence of 5.4%. This is far higher than values stated in multiple studies notably in the USA by Pollock et al in 2010 and in Nigeria by Ozumba et al in 2018 [8-13], who identified frequencies varying between 0.2% and 1.6 %. In their studies, patients were solely recruited in the intensive care unit. Whereas, some patients presented hemodynamic instability but did not meet the criteria for admission in the intensive care unit [26]. Our incidence could have been lower if it was obtained solely from patients admitted in the intensive care unit. Whereas, in our survey,, patients were equally recruited in other units such as the labor room and emergency ward. Their hemodynamic state were stabilized without needing admission into the intensive care unit. Another reason for the differences is the study duration. We conducted our study in 5months compared to other studies with durations of 5years period. The longer the study period is, the larger the denominator (number of delivery) hence the smaller the incidence.
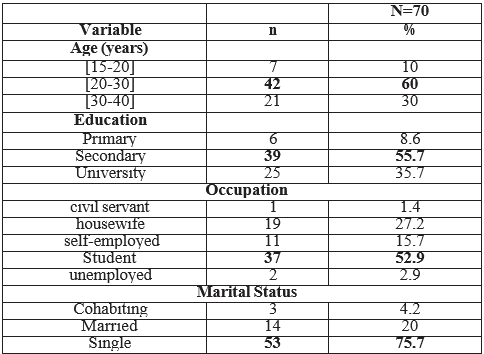
The most represented group in our study were those aged between 20 to 30 years in 60% of cases with a mean maternal age of 27.3 ±5.2 years. This is similar to results obtained by Ozumba et al in 2018 in Nigeria and Dasgupta et al in 2017 in India [12,13], but studies from abroad report a higher maternal age with a mean age of 31.8 (+/-5.76) years which is consistent with birth age patterns in developed countries [27,28] (Table 1).
Most of our patients were students in 52.9% and had a secondary educational level 55.7% and were single 75.7%.This is similar to that obtained by Soares et al in 2020 [16]. Higher level of education appears protective against maternal mortality. This is in accordance with previous publications showing a relationship between lower level of education and a higher likelihood of maternal death; less‐educated women present at a hospital later and in a more severe condition [29]. Equally, students are most often financially dependent and unstable hence they may lack the financial resources to ensure proper antennal booking.
The majority of patients were single (75.7%). This correlates with the high frequency of students in our study. Students are most likely to get married at a later age. According to literature review, the RR of unmarried women was highest for abortions, ectopic pregnancies, and antepartum hemorrhage (combined RR 2·98 [2·11–4·19]) compared to married women [30]. This may equally be due to the fact that, unmarried women most often lack emotional and financial support and have poor health behaviors [31], hence leading to higher rate of unwanted pregnancies, abortions and other complications of pregnancies.
Clinical variables of obstetric hemodynamic instability The majority of our study participants were primiparous and pauciparous in 35.7% and 44.3% respectively. This is similar to data obtained by Dasgupts et al in 2017 in India and Soares et al in 2020 [12,16]. Bhat et al in India in 2013 reported higher percentage of multiparous patients [32]. The difference is probably due to the correlation with a high percentage of single patients being diagnosed with complications of pregnancy-induced hypertension. Given that primiparity is a known risk factor of pregnancy induced hypertension. The majority of cases where diagnosed during pregnancy in 82.9%. This is different from data obtained by Dasgupts et al who reported higher frequency of post-partum cases. This difference could be as a result of the correlation between higher frequency of single patients and unwanted pregnancies both leading to complications such as abortion, ectopic pregnancies and antepartum hemorrhage [30].
Most of our patients were unbooked or poorly booked for antenatal care in 38.6% and 44.3% respectively. Ozumba et al in 2018 in Nigeria reported similar results [13]. The low socio-economic status could favor this situation. Un-booked or poorly booked patients were more likely to have adverse pregnancy outcomes.
Our study revealed a mean obstetric shock index of 1.12 bpm/mmHg. Through the literature review, we found an obstetric shock index in pregnant women greater than 0.9 bpm/mmHg, increased the risk of poor maternal outcome and of receiving blood transfusion [5,33]. However, obstetric shock index accurately estimate the degree of visible and invisible (i.e. intra-peritoneal or bleeding into paravaginal tissue) blood loss as well.
The majority of patients consulted 6hrs after the onset of symptoms in 62.9% of cases. It has been demonstrated by Rodolfo et al in Brazil and Hiros et al in the united states of America, that any form of consultation delay was significantly associated with adverse maternal outcome [34,35]. The increased frequency of delay correlates with the high frequency of un-booked or poorly booked patients, resulting from lack of consciousness and patient information over emergency signs warranting early consultation. However, this could also be related with difficulties to access appropriate health facilities due to financial constraints.
Etiologies of obstetric hemodynamic instability In our study, by order of preference obstetric hemorrhage was the most frequent cause of obstetric hemodynamic instability with 65.7%, followed by pregnancy-induced hypertension in 17.1%, obstetric sepsis in 14.3% and pulmonary embolism in 2.9%. These results correlates with that obtained by Ozumba et al in 2018 in Nigeria and Dasgupta et al in 2017 in India [12,13]. The most common primary diagnosis leading to critical care admission has hovered between obstetric hemorrhage and pregnancy- induced hypertension in multiple studies [12-36]. According to CDC and WHO, theses etiologies remained the primary cause of maternal morbidity and mortality [15]. The specific causes of obstetric hemorrhage were ruptured ectopic pregnancy (15.7%), post- partum hemorrhage (14.3%), incomplete abortion (12.9%), antepartum hemorrhage (10%) and uterine rupture (8.6 %). Our study population was mostly made of single students, primiparous and pauciparous, with a mean gestational age of 22weeks. This could probably explain the high frequency of pregnancy-induced hypertension, ruptured ectopic pregnancy and abortion (Figures 1,2).
Discussion:
Cesarean session and laparotomy were the most frequent surgical treatment used in 40.3% and 38.2% respectively to manage the causes of obstetric hemodynamic instability. This was owing to the predominant admission of obstetric surgical emergencies notably antepartum hemorrhage, ruptured ectopic pregnancy, uterine rupture. These findings are similar to Ozumba et al results [13]. However fewer patients (20.4%) were treated with antihypertensive and anti- convulsant. All our patients were placed on antibiotics. Oxygen supplementation and blood transfusion were also required in majority of the patients (62.9% and 77.1% respectively).
This may also be as a result of the mode of presentation and the clinical indication for admission. The majority of our patients (75.7%) were referred from health centers after being consulted by less competent health care worker. Majority without an intravenous line (60.9%). The poor health‑seeking behavior of patients, late referral, coupled with low socioeconomic status of patients could have delayed the management, hence complicating their clinical state. This correlates with other findings in our study as majority of patients consulted 6hrs after the onset of symptoms in 62.9% of cases and majority of patients received treatment 1hr after consultation. In effect, a review of the literature enabled to underline the fact that any form of delay was significantly associated with adverse maternal outcome [34,35].
Factors of poor maternal outcome After univariate logistic regression, we found an association between marital status and maternal outcome. The risk of having an unfavorable outcome increased by 5 [OR=4.6; CI (0.41-103.81); p-value =0.0088] in unmarried patients. The majority of patients (75.7%) were single. This correlates with the high frequency of students in our study, indicating a tendency to get married at a later age. This may equally be due to the fact that, unmarried women most often lack emotional and financial support and have poor health behaviors hence leading to higher rate of unwanted pregnancies, abortions and other complications of pregnancies [31]. According to literature review, the RR of unmarried women was highest for abortions, ectopic pregnancies, and antepartum hemorrhage [combined RR 2·98 (2·11–4·19)] compared with married women [30].
A delay of more than six hours between the onset of symptoms and consultations, multiplied the risk by [OR=2.6; CI (0.5, 18.8); p- value=0.0463] the possibility of having an unfavorable outcome likewise, a delay of more than one hour between consultation and management multiplied the risk of poor maternal outcome by 3 [OR=3.3; CI (0.98, 28.9); p-value=0.0005]. This has been demonstrated by Rodolfo et al in Brazil and Hiros et al in the united states of America, that any form of delay was significantly associated with adverse maternal outcome [34,35]. The poor health‑seeking behavior of patients, late referral from health centers and low socioeconomic status of patients could delay the management, hence complicating patient’s clinical state.
Being consulted by a midwife in a health center increased the risk for hemodynamic instability [OR=8.6; C.I (2.2, 43.2); p-value=0.0036]. This could be explained by the fact that they may be less skilled to properly diagnose pathologies, this causing misdiagnosis and delayed appropriate management. Patients with obstetric shock index of 0.98 and above, were equally more at risk for hemodynamic instability [OR=4.04; C.I (0.98, 88.7); p-value=0.0535]. As described in the literature, an obstetric shock index in pregnant women greater than 0.9 bpm/mmHg, effectively increases the risk of poor maternal outcome and of receiving blood transfusion as found in our survey [5,33]. More over, obstetric shock index accurately estimates the degree of visible and invisible (i.e. intra- peritoneal or bleeding into paravaginal tissue) blood loss.
On the other hand, patients who had ≥4 antenatal consultations had lesser chances of unfavorable outcome [OR=0.9; CI (0.14, 7.01; p- value=0.0491]; p-value=0.0491). According to Ozumba in Nigeria un- booked or poorly booked patients were more likely to have adverse pregnancy outcomes [13]. Whereas, the WHO recommends at least 8 antenatal care visits which implies adequate antenatal consultations with appropriate exposure to health care providers and information on alarm and danger signs during perinatality [37].
Conclusion
Hemodynamic instability is very frequent in our setting. It occurs mostly in young single adults and mostly students who have a secondary educational level. They are mostly primiparous and pauciparous and are poorly booked for antenatal care. They are often referred from health centers without an intravenous line and the majority of patients consult six hours after the being onset of symptoms and receive their first treatment more than an hour after their first consultation. Obstetric hemorrhage is the most frequent cause of obstetric hemodynamic instability with the majority having a favourable outcome. Nevertheless, obstetric hemodynamic instability accounted for one fifth of maternal demise. The probable factors of poor maternal outcome were unmarried patients, a delay of more than six hours between the onset of symptoms and consultation, a delay of more than one hour between consultation and management, being consulted by a mid-wife, an obstetric shock index of 0.98 and above. Therefore,there is need to develop standardized monitoring protocols in all medical structures for the early identification of precocious maternal warning signs. This may comprise a number of useful preventive measures, such as the implementation of early maternal warning system chart and obstetric shock index as clinical tools. Furthermore, improvements with timely and appropriate patients’ referral and booking may render the holistic management of obstetric hemodynamic instability more efficient.
References
-
Kramer KJ (2018) Hemodynamic Instability as a Complication of Maxillofacial Surgery: Ferneini EM, Bennett JD, editors. Perioperative Assessment of the Maxillofacial Surgery Patient: Problem-based Patient Management: Springer International Publishing. 579-593.
View at Publisher | View at Google Scholar -
NICE (2014) The hTEE system for transoesophageal echocardiographic monitoring of hemodynamic instability [Internet]. Medtech innovation.
View at Publisher | View at Google Scholar -
Hanqing Cao, Eshelman L, Chbat N, Nielsen L, Gross B, et al. (2008) Predicting ICU hemodynamic instability using continuous multiparameter trends. In: 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2008: 3803-3806.
View at Publisher | View at Google Scholar -
Sevransky J (2009) Clinical Assessment of Hemodynamically Unstable Patients. Curr Opin Crit Care. 15: 234-238.
View at Publisher | View at Google Scholar -
Rojas-Suarez J, Borré D, Zapata R (2021) Hemodynamic Monitoring of the Critically Ill Obstetric Patient. Lapinsky S editor. The continuous textbook of Women’s medicine series- obstetrics module-vol-9 principles and practice of obstetric high- dependency and critical care, Glob. libr. Women’s med.
View at Publisher | View at Google Scholar -
Buitenwerf E, Boekel MF, van der Velde MI, Voogd MF, Kerstens MN, et al. (2019) The haemodynamic instability score: Development and internal validation of a new rating method of intra-operative haemodynamic instability. Eur J Anaesthesiol EJA. 36: 290-296.
View at Publisher | View at Google Scholar -
Mehdi M, Chandraharan E (2021) Diagnosis and Management of Shock in Postpartum Hemorrhage. Fernanda Escobar MV editor. The continuous textbook of Women’s medicine series-obstetrics module-vol-13 obstetric emergency, Glob libr Women’s med.
View at Publisher | View at Google Scholar -
Pollock W, Rose L, Dennis CL (2010) Pregnant and postpartum admissions to the intensive care unit: a systematic review. Intensive Care Med. 36: 1465-1474.
View at Publisher | View at Google Scholar -
Kilpatrick SJ, Matthay MA (1992) Obstetric Patients Requiring Critical Care. Chest. 101: 1407-1412.
View at Publisher | View at Google Scholar -
Zwart JJ, Dupuis JRO, Richters A, Ory F, van Roosmalen J (2010) Obstetric intensive care unit admission: a 2-year nationwide population-based cohort study. Intensive Care Med. 36: 256-263.
View at Publisher | View at Google Scholar -
Vargas M, Marra A, Buonanno P, Iacovazzo C, Schiavone V, et al. (2019) Obstetric Admissions in ICU in a Tertiary Care Center: A 5-Years Retrospective Study. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 23: 213-219.
View at Publisher | View at Google Scholar -
Dasgupta S, Jha T, Bagchi P, Singh SS, Gorai R, et al. (2017) Critically Ill Obstetric Patients in a General Critical Care Unit: A 5 Years’ Retrospective Study in a Public Teaching Hospital of Eastern India. Indian J Crit Care Med. 21: 294-302.
View at Publisher | View at Google Scholar -
Ozumba BC, Ajah LO, Obi VO, Umeh UA, Enebe JT, et al. (2018) Pattern and Outcome of Obstetric Admissions into the Intensive Care Unit of a Southeast Nigerian Hospital. Indian J Crit Care Med. 22: 16-19.
View at Publisher | View at Google Scholar -
ACOG Practice Bulletin No. 211: Critical Care in Pregnancy. Obstet Gynecol. 133: e303-319.
View at Publisher | View at Google Scholar -
NIH (2020) What are examples and causes of maternal morbidity and mortality?
View at Publisher | View at Google Scholar -
Soares FM, Pacagnella RC, Tunçalp Ö, Cecatti JG, Vogel JP, et al. (2020) Provision of intensive care to severely ill pregnant women is associated with reduced mortality: Results from the WHO Multicountry Survey on Maternal and Newborn Health. Int J Gynecol Obstet. 150: 346-353.
View at Publisher | View at Google Scholar -
Richard E Klabunde (2013) CV Physiology | Hypotension – Introduction.
View at Publisher | View at Google Scholar -
Trikha A, Singh PM (2018) Management of major obstetric haemorrhage. Indian J Anaesth. 62: 698-703.
View at Publisher | View at Google Scholar -
Hook V (2014) Acute Kidney Injury During Pregnancy. Clin Obstet Gynecol. 57: 851-861.
View at Publisher | View at Google Scholar






