Case Report | DOI: https://doi.org/IJCCRI-CR-24-006
Mobile Teledermatology Update 2 Of Different Clinical Cases Presentation
Abstract
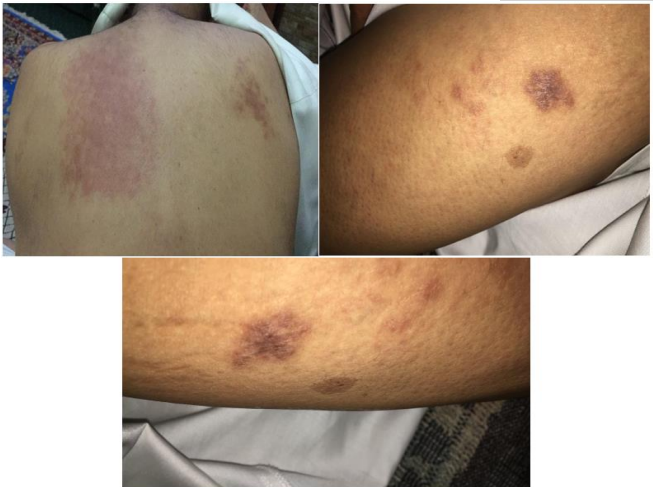
Background: Teledermatology involves a qualified professional clinical photographer taking a series of digital photographs of a patient's skin lesion. The photographs are then sent to a dermatologist for remote assessment to see if the patient needs to come into hospital for further treatment.
Objective: To study the pattern of cutaneous clinical cases sent through social media Patients and Methods males and females’ infants and children's and adults patients presented and sent photos through Whatsapp with different clinical skin lesions
Results: The clinical data and the information about the patients showed they had different skin diseases.
Conclusion: Now a days social media solved many things in internet and the far is near. All Those neam from ALLAH. Alhamdolellah Spotting diagnosis and the treatment and follow up performed free of charge.
Introduction
Teledermatology is a subspecialty in the medical field of dermatology and probably one of the most common applications of telemedicine and e-health.[1] In teledermatology, telecommunication technologies are used to exchange medical information (concerning skin conditions and tumors of the skin) over a distance using audio, visual, and data communication. Applications comprise health care management such as diagnoses, consultation, and treatment as well as (continuous) education.
The dermatologists Perednia and Brown were the first to coin the term "teledermatology" in 1995. In a scientific publication, they described the value of a teledermatologic service in a rural area underserved by dermatologists Mobile telemedicine is a system in which at least one participant (the person seeking advice or the doctor, for instance) uses wireless or mobile equipment i.e. mobile phones, handheld devices), in contrast to conventional stationary telemedicine platforms. Travelers who develop skin lesions as well as doctors who are on the move in hospital/non-hospital area can benefit from this new development in teledermatology. To facilitate access to medical advice and enable individuals to play a more active role in managing their own health status, mobile teledermatology seems to be especially suited for patient filtering or triage. (i.e. referral based on the severity and character of their skin condition). Another possible practical application is for follow-up of individuals with chronic skin conditions. However, currently available studies show a high rate of missed skin cancers including melanoma, and there is not enough robust data to recommend this method of diagnosis and treatment. Suitability of cases Not all cases are suitable for teledermatology. The type of cases .suited for teledermatology is a topic, which requires more studies. Some studies have observed that eczema and follicular lesions were diagnosed with relatively more certainty, while in some other studies it was seen that diagnoses were made with more certainty in cases like viral warts, herpes zoster, acne vulgaris, irritant dermatitis, vitiligo, and superficial bacterial and fungal infections. Implemented projects by country of Yemen.









References
-
^ Wootton R (December 2017).
View at Publisher | View at Google Scholar -
^ Wurm EM, Hofmann-Wellenhof R, Wurm R, Soyer HP (February 2008).
View at Publisher | View at Google Scholar -
^ Burg G, Soyer HP, Chimenti S (2005).
View at Publisher | View at Google Scholar -
^ Perednia DA, Brown NA (January 1995).
View at Publisher | View at Google Scholar -
^ Chuchu, Naomi; Dinnes, Jacqueline; Takwoingi, Yemisi; Matin, Rubeta N; Bayliss, Susan E; Davenport, Clare; Moreau, Jacqueline F; Bassett, Oliver; Godfrey, Kathie; O'Sullivan, Colette; Walter, Fiona M (4 December 2018). Cochrane Skin Group (ed.).
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^ Binder B, Hofmann-Wellenhof R, Salmhofer W, Okcu A, Kerl H, Soyer HP (December 2007).
View at Publisher | View at Google Scholar -
^ Ford, Adam R.; Gibbons, Caitlin M.; Torres, Josefina; Kornmehl, Heather A.; Singh, Sanminder; Young, Paulina M.; Chambers, Cindy J.; Maverakis, Emanual; Dunnick, Cory A.; Armstrong, April W. (2019).
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^ Massone C, Soyer HP, Lozzi GP, Di Stefani A, Leinweber B, Gabler G, et al. (April 2007).
View at Publisher | View at Google Scholar -
^ * Bauer J, Leinweber B, Metzler G, Blum A, Hofmann-Wellenhof R, Leitz N, et al. (September 2006).
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^ Snoswell C, Finnane A, Janda M, Soyer HP, Whitty JA (June 2016).
View at Publisher | View at Google Scholar -
^ Chuchu N, Takwoingi Y, Dinnes J, Matin RN, Bassett O, Moreau JF, et al. (December 2018).
View at Publisher | View at Google Scholar -
^ * Kaliyadan F, Venkitakrishnan S (2009).
View at Publisher | View at Google Scholar -
^ Schofield J, Grindlay D, Williams H. Skin conditions in the UK: a health care needs assessment. Nottingham: Centre of Evidence Based Dermatology, University of Nottingham, 2009.
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^
View at Publisher | View at Google Scholar -
^ von Wangenheim A, Nunes DH (2019).
View at Publisher | View at Google Scholar -
^ Giavina Bianchi M, Santos A, Cordioli E (2021).
View at Publisher | View at Google Scholar -
^ Snoswell CL, Caffery LJ, Whitty JA, Soyer HP, Gordon LG (June 2018).
View at Publisher | View at Google Scholar -
^ Snoswell CL, Whitty JA, Caffery LJ, Finnane A, Soyer HP (August 2019).
View at Publisher | View at Google Scholar






