Case Report | DOI: https://doi.org/CCSRR-CR-25-013
Massive Pulmonary Embolism with Right Atrial Thrombus: A Case Report
Abstract
We present a unique case of a 53-year-old woman who was admitted to the emergency department with acute dyspnea persisting for 24 hours. Despite initial hemodynamic stability, a diagnostic workup revealed a massive pulmonary embolism (PE) involving both pulmonary arteries and multiple thrombi within the right atrium (RA), an uncommon and high-risk presentation. Elevated D-dimer levels, computed tomography pulmonary angiography (CTPA), and transthoracic echocardiography (TTE) confirmed the diagnosis. The patient was treated successfully with anticoagulation therapy, leading to significant clinical improvement. This case is unique due to the simultaneous presence of right atrial thrombi and massive PE in a patient without traditional risk factors such as atrial fibrillation, malignancy, or recent surgery. The management approach focused on anticoagulation therapy, highlighting the importance of individualized treatment in complex cases. This report underscores the need for a comprehensive diagnostic workup and multidisciplinary management in rare and challenging presentations of PE.
Introduction
Pulmonary embolism (PE) is a common and potentially life-threatening condition caused by the obstruction of the pulmonary arteries, usually due to thrombi originating from the deep veins of the lower extremities . The clinical presentation of PE can vary widely, ranging from asymptomatic cases to severe, life-threatening events such as massive PE, which is associated with significant morbidity and mortality . In rare cases, emboli may originate from thrombi located in the right atrium (RA), complicating the clinical picture and posing additional therapeutic challenges .
This case report discusses the diagnosis and management of a patient with a massive pulmonary embolism complicated by the presence of multiple right atrial thrombi, underscoring the importance of early recognition and multidisciplinary management in such cases. It highlights the importance of considering RA thrombi in the differential diagnosis of PE, especially in patients without traditional risk factors like atrial fibrillation, malignancy, or recent surgery .
Case Presentation
A 53-year-old woman presented to the emergency department with a sudden onset of dyspnea that had persisted for approximately 24 hours. She reported no chest pain, hemoptysis, or palpitations. The patient described feeling anxious due to the worsening of her symptoms but denied any recent history of trauma, surgery, or prolonged immobilization. She had no significant medical history of thromboembolic events, chronic illnesses, or hormone replacement therapy use. On physical examination, the patient appeared anxious but hemodynamically stable. Her vital signs revealed a blood pressure of 125/80 mmHg, a heart rate of 88 beats per minute, a respiratory rate of 22 breaths per minute, and an oxygen saturation of 94% on room air. She was afebrile, with a temperature of 98.6°F (37°C). Cardiovascular examination showed a regular heart rhythm with no signs of heart failure. Respiratory examination revealed mild wheezing and decreased breath sounds at the bases, but no crackles or pleural rubs. The rest of her systemic examination was unremarkable.
Given her acute dyspnea and clinical findings, a preliminary diagnosis of PE was considered. Laboratory investigations showed an elevated D-dimer level of 1973 ng/mL (normal range < 500>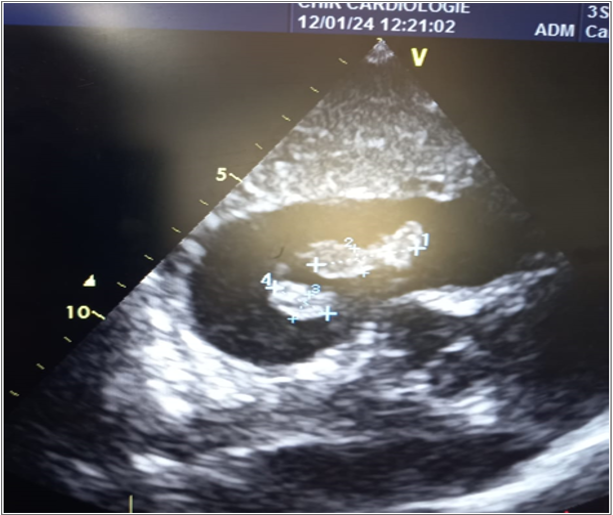
Upon confirmation of a massive PE with concomitant right atrial thrombi, the patient was stabilized with supplemental oxygen. Anticoagulation therapy was initiated with intravenous heparin to prevent further thrombus formation and reduce the risk of embolization. The presence of multiple right atrial thrombi posed a significant risk of further embolization to the pulmonary circulation. A multidisciplinary team of cardiologists, pulmonologists, and hematologists was consulted to devise an appropriate management plan.
Given the patient's stable hemodynamic status and the risk of bleeding associated with thrombolytic therapy, the decision was made to forgo thrombolysis and proceed with anticoagulation therapy alone. The patient was closely monitored, and her condition showed steady improvement with anticoagulation. Her dyspnea decreased, and her oxygen saturation improved to 98% on room air. Repeat echocardiography performed 48 hours later showed a reduction in the size of the right atrial thrombi and decreased right ventricular strain. A follow-up CTPA confirmed partial resolution of the pulmonary embolism.
The patient was transitioned to oral anticoagulation with warfarin, with a target INR of 2-3, and was monitored for bleeding or other complications. She was advised to continue anticoagulation therapy for at least six months. The patient was discharged with follow-up plans, including regular echocardiographic evaluations and INR monitoring.
Discussion
This case emphasizes the importance of early diagnosis and management of massive pulmonary embolism, particularly when complicated by the presence of right atrial thrombi. PE is often challenging to diagnose due to its nonspecific presentation . Elevated D-dimer levels can be helpful in screening for thromboembolic events , and imaging studies such as CTPA and echocardiography are crucial for confirming the diagnosis and assessing the extent of thromboembolic disease .
The presence of right atrial thrombi in the context of PE is rare but increases the risk of further embolization and adverse outcomes. Right atrial thrombi may develop in situ, especially in patients with conditions like atrial fibrillation or heart failure , although our patient had none of these risk factors. Anticoagulation therapy is typically the mainstay of treatment for PE with right atrial thrombi, and in this case, it was sufficient to manage the thrombus burden without the need for thrombolysis .
The decision to forgo thrombolytic therapy in favor of anticoagulation was based on the patient's stable condition and the associated risks of bleeding with thrombolysis . This case supports the use of anticoagulation alone in selected patients with massive PE and right atrial thrombi, particularly when thrombolysis may pose additional risks .
Conclusion
Massive pulmonary embolism with right atrial thrombus is a rare but potentially life-threatening condition that requires prompt diagnosis and management. This case underscores the importance of considering right atrial thrombi in patients presenting with massive PE. A comprehensive diagnostic approach, including imaging studies such as CTPA and echocardiography, is crucial in identifying the presence of thrombi and assessing the extent of thromboembolic disease. Early initiation of anticoagulation is essential for improving patient outcomes. Multidisciplinary collaboration is vital in managing complex cases of thromboembolic disorders, as demonstrated in this case report.
No acknowledgment.
The patient's consent has been obtained for the writing and publication of this case report.
The author declares no conflicts of interest.
References
-
Cao Y, Geng C, Li Y, Zhang Y. In situ Pulmonary Artery Thrombosis: A Previously Overlooked Disease. Front Pharmacol. 2021 Jul 8;12:671589.
View at Publisher | View at Google Scholar -
Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism. Exp Clin Cardiol. 2013 Spring;18(2):129-38. PMID: 23940438;
View at Publisher | View at Google Scholar -
Susilo H, Julario R, Dyah Kencono Wungu C. Case Report: Successful revascularization in massive pulmonary embolism with a large protruding thrombus and dilated cardiomyopathy. F1000Res. 2021 Jan 11;10:13.
View at Publisher | View at Google Scholar -
Degiovanni A, Carassia C, De Vecchi S, Erbetta R, Patti G. Atrial thrombosis: Not only left, think also about right! J Clin Ultrasound. 2022 Oct;50(8):1194-1201. doi: 10.1002/jcu.23311. PMID: 36218213
View at Publisher | View at Google Scholar -
Schellhaass A, Walther A, Konstantinides S, Böttiger BW. The diagnosis and treatment of acute pulmonary embolism. Dtsch Arztebl Int. 2010 Aug;107(34-35):589-595.
View at Publisher | View at Google Scholar -
Himeno M, Nagatomo Y, Miyauchi A, Sakamoto A, Kiyose K et al. D-Dimer beyond Diagnosis of Pulmonary Embolism: Its Implication for Long-Term Prognosis in Cardio-Oncology Era. J Pers Med. 2023 Jan 27;13(2):226.
View at Publisher | View at Google Scholar -
Oh JK, Park JH. Role of echocardiography in acute pulmonary embolism. Korean J Intern Med. 2023 Jul;38(4):456-470.
View at Publisher | View at Google Scholar -
Right atrial thrombi may develop in situ, especially in patients with conditions like atrial fibrillation or heart failure (Jaff et al., 2011)
View at Publisher | View at Google Scholar -
Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part II: Management. Exp Clin Cardiol. 2013 Spring;18(2):139-147.
View at Publisher | View at Google Scholar -
Zuo Z, Yue J, Dong BR, Wu T, Liu GJ, Hao Q. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev. 2021 Apr 15;4(4):CD004437.
View at Publisher | View at Google Scholar -
Condliffe R, Elliot CA, Hughes RJ, Hurdman J, Maclean RM, Sabroe I, van Veen JJ, Kiely DG. Management dilemmas in acute pulmonary embolism. Thorax. 2014 Feb;69(2):174-180.
View at Publisher | View at Google Scholar






