Review Article | DOI: https://doi.org/IJCCRI-RW-24-011
Imaging errors- Catastrophes in Clinical Diagnosis! Has Potential to Improve Diagnostic Performance- a Missed Opportunity
Abstract
Medical imaging is crucial for diagnosing and monitoring a wide range of conditions, from simple bone fractures, pregnancies to complex diseases like Brain damage, cancer and cardiovascular diseases. Imaging plays a pivotal role in the diagnostic process for many patients. The global medical imaging market size was at $40.33 billion in 2023 and is projected to reach $49 billion in 2024 and reach $75 billion by 2032, growing at a compound annual growth rate (CAGR) of 6.4% [1]. With an average diagnostic error rates of 5%, there would be approximately 50 million diagnostic errors involving imaging annually worldwide. The potential to improve diagnostic performance and reduce patient harm by identifying and learning from these errors is substantial.
Karnataka State Commission (KSCDRC) 0n 12 November 2024, ordered a Radio-Diagnostic Centre in Bengaluru, to compensate a woman for a misdiagnosis leading to unnecessary surgery for Tubal Pregnancy and missing a normal Pregnancy after a gap of 12 years. This is an eye opener decision for at educated families in Urban India not to accept blunders of Diagnostic facilities.
Unfortunately, the greater understanding of error–its frequency and to a certain extent its inevitability–which radiologists have gained over the past two decades is not shared even by colleagues in our own profession who often seem to have unrealistic expectations of the accuracy of radiological interpretation.
One of the biggest problems facing radiologists now is the yawning gap between what we know to be our error rate and what our patients might believe it to be.
Developing a comprehensive process to identify diagnostic errors, analyse them to discover contributing factors and biases, and develop interventions based on the contributing factors is fundamental to learning from diagnostic errors.
Materials and Methods: This article uses the example of a recent Karnataka State Consumers Redressal Commission (KSCDRC)’s order of 12 November 2024, against a Radio-Diagnostic Centre in Bengaluru of misdiagnosis of a Tubal Pregnancy leading to a courageous litigation over 12 years supported by literature review
Outcome: Though the litigant is compensated for the ordeal over 12 years, there is no learning for the profession in developing interventions based on the contributing factors and pave way for learning from diagnostic errors in the Imaging profession.
Introduction:
Karnataka State Commission (KSCDRC) 0n 12 November 2024, ordered a Radio-Diagnostic Centre in Bengaluru, to compensate a woman for a misdiagnosis leading to unnecessary surgery for Tubal Pregnancy [1].
A diagnostic approach is a method or test used to help diagnose a disease or condition. It involves multiple steps like i) Initial assessment: Taking the patient's history, performing a physical exam, and evaluating their symptoms ii) Making Provisional diagnosis or differential diagnosis iii) Initiation of primary treatment to address urgent relief of main complaints like pain, fever, itching etc. iv) Simultaneously ordering tests: Administering diagnostic tests to help determine the cause of the illness v) Reviewing the supportive data: Analysing the test results and corroborate clinical findings to come to a diagnosis vi) Finally deciding treatment based on the diagnosis vii) Monitoring the prognosis and determining the next steps for treatment or further testing. Common diagnostic techniques include measuring blood pressure, pulse, and temperature, looking tongue and lips for pallor, Blood or Serological Biomarker tests, Imaging tests [2,3].
Medical imaging is crucial for diagnosing and monitoring a wide range of conditions, from simple bone fractures, pregnancies to complex diseases like Brain damage, cancer and cardiovascular diseases. Imaging plays a pivotal role in the diagnostic process for many patients. The global medical imaging market size was at $40.33 billion in 2023 and is projected to reach $49 billion in 2024 and reach $75 billion by 2032, growing at a compound annual growth rate (CAGR) of 6.4% [4,5]. Evidence from the plain film era suggested a radiologist error rate of around 5% in daily practice. Now, the rates of interpretative error in cross-sectional imaging are significantly higher, of the order of 20–30%. Even with an average diagnostic error rates of 5%, there would be approximately 50 million diagnostic errors involving imaging annually worldwide [5].
Most errors especially in Rural India go un-reported, under reported or covered up and even refuted by the imaging centres or Health Insurance companies. And even if they are brought to legal authorities like Consumer Redressal System, the biggest achievement is as awarding some compensation to the patients and punitive action on the professional concerned, that too after a decade’s legal battle. What is desirable is the honest efforts of learning by the professionals to avoid such blunders in future.
Relatively high diagnostic error rates have persisted in the medical diagnostic field despite decades of research and interventions. It may seem as if diagnostic errors in radiology occur in a haphazard fashion, but not so, they are predictable events with readily identifiable contributing factors, many of which are or related to the external environment. The potential to improve diagnostic performance and reduce patient harm by identifying and learning from these errors is substantial.
The discovery in hindsight of an error in interpretation of a radiological image is now commonplace in our practice but is still often perceived by the patient as something shocking and exceptional, calling into question the competence of the radiologist involved.
It will not be easy. “Technical” solutions such as a process of consent prior to imaging or disclaimers on reports are unlikely to be popular or effective. The pervasive nature of radiological error as well as the measures which can be taken to avoid, despite its inherent flaws–must continue to bring to patient care [5].
This article is an effort to stress the need to develop a comprehensive process to identify diagnostic errors, analyse them to discover contributing factors and biases, and develop interventions based on the contributing factors and pave way for fundamental to learning from diagnostic errors in the Imaging profession.
Awarding Compensation to a case of Misdiagnosed Tubal Pregnancy after a decade.:
Ms. Lavanya (name changed) aged 24 years married for about a year, approached her family physician for missed periods for 8 weeks, and abdominal discomfort. She in-turn referred her to Tertiary care specialist hospital where an Obstetrician after physical examination, referred for all routine examinations (Urine, Blood etc.) and an Ultrasonography in August 2012. The Ultrasonologist report read “A right tubal Pregnancy”. The obstetrician fearing tubal rupture an emergency condition, did an elective Laparotomy surgery the same day.
On opening the abdomen, she did not find any tubal pregnancy, instead a small cyst in the left fimbriae region was found which was removed. A week later a repeat scanning was done in a different diagnostic centre, which confirmed a normal intra-uterine pregnancy. The pregnancy continued normally, and the lady delivered a male baby in due course, but the entire events costed the family over INR.100,000.
After confirmation of a normal delivery the family filed a case in Additional district consumer disputes redressal commission, alleging that the first diagnostic centre had failed to provide accurate findings, constituting a clear deficiency in service. The Centre gave a false statement saying that neither they did and test nor gave a report, but the district consumer disputes redressal commission awarded INR 15,000 in compensation on 8 July 20213.
However, dissatisfied with the award the family appealed to Karnataka State Consumer Disputes Redressal Commission (KSCDRC), saying that the compensation was inadequate for the mental agony she had to undergo and other ordeals of reaching other institutions, though all ended in normal delivery. The state commission, after reviewing the case inferred that the first diagnostic centre was guilty of a deficiency of service, as the institution’s report of Right Tubal pregnancy was in contradiction of subsequent finding within a week. The Commission also commented that the misdiagnosis caused unnecessary surgery, failing to give in creditable explanation for the incorrect diagnosis. The ordeal for the patient and the family, can’t be compensated in anyway. Reprimanding the district Redressal commission for compensating a meagre amount after inferring that the complaint had failed to prove deficiency of service on the part of the diagnostics centre. Latest order gets a compensation of INR 50,000 with a 9% annual interest along with litigation cost.
Discussions:
A diagnostic approach is a method or test used to help diagnose a disease or condition. It involves multiple steps like i) Initial assessment: Taking the patient's history, performing a physical exam, and evaluating their symptoms ii) Making Provisional diagnosis or differential diagnosis iii) Initiation of primary treatment to address urgent relief of main complaints like pain, fever, itching etc. iv) Simultaneously ordering tests: Administering diagnostic tests to help determine the cause of the illness v) Reviewing the supportive data: Analysing the test results and corroborate clinical findings to come to a diagnosis vi) Finally deciding treatment based on the diagnosis vii) Monitoring the prognosis and determining the next steps for treatment or further testing. Common diagnostic techniques include measuring blood pressure, pulse, and temperature, looking tongue and lips for pallor, Blood or Serological Biomarker tests, Imaging tests [2].
A good clinician makes any diagnosis by Pattern recognition, Algorithm, Inductive method, and Hypothetico-deductive method. Diagnosis has important implications for patient care, research, and policy. It is both a process and a classification scheme, or a “pre-existing set of categories agreed upon by the medical profession to designate a specific condition.”
When a diagnosis is accurate and made in a timely manner, a patient has the best opportunity for a positive health outcome because clinical decision making will be tailored to a correct understanding of the patient's health problem. In Health administration of a facility or State /Country public policy decisions are influenced by diagnostic information, such as setting payment policies, resource allocation decisions, and research priorities [2,3]
In the diagnostic process, the roles of diagnostic uncertainty and time mount the complexity of health care, due to the ever-increasing options for diagnostic testing and treatment. The rapidly rising levels of Imaging, biomedical and clinical evidence to inform clinical practice, and the frequent comorbidities among patients due to the aging of the population are becoming more complex in the last 2 decades. Clinicians are relying more on diagnostics that their clinical acumen due mainly to the rising complexity of health care and the sheer volume of advances, coupled with clinician time constraints and cognitive limitations, have outstripped human capacity to apply this new knowledge. The role of clinical practice guidelines in informing decision making in the diagnostic process is being accorded second preference and creating more diagnostic evidence. The issue is in such cases if there is a misdiagnosis at the Laboratories and imaging centre based on which the treating doctor intervenes and does something who must be held accountable and must compensate the patient or the family [3].
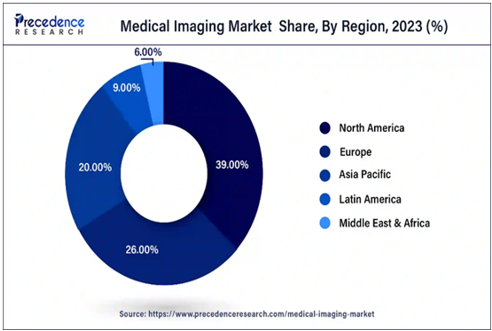
Diagnostic errors include missed, delayed, and wrong diagnosis, as well as failure to communicate the diagnosis effectively to the patient and family members. Interventions to improve diagnostic testing should target breakdowns in the testing process that lead to diagnostic error and technical clarifications of what went wrong and sharing them widely so that others can learn from such mistakes apart from compensation to the patient and A simple way to conceptualize diagnostic errors in the testing process is to classify them as preanalytical, analytic, or postanalytical [5]. Global magnitude of imaging market is highest in developed countries like USA, Europe followed by Asia Specific, Latin America and Middle and East Africa. The medical imaging market in India is fast growing and vibrant. Given the inherent layered nature of the Indian market, there is demand for value, mid-tier as well as premium offerings, driven by corporate & private hospitals. We are witnessing an increasing contribution by the public sector at districts, state as well as the centre aided by various health insurance schemes such as Ayushman Bharat.
Latest technological advancements have completely disrupted the way healthcare was being offered and consumed so far. The latest technologies that are currently shaping medical imaging space are bedside imaging products, telehealth solutions, cloud-based applications, image fusion, Realtime imaging, 3D imaging technology and advances in storage & retrieval of imaging data. Also, artificial intelligence (AI) solutions are playing a far more important role than ever before by aiding radiologists to spot anomalies in human tissues for multiple disease conditions.
Medical Imaging has a bright future in our country with steady growth driven by domestic and foreign players. Increased access, adoption by trained Health Care Providers, awareness, and affordability (through private and government insurance) will allow the market grow exponentially. Going forward, Products and solutions integrated with Artificial Intelligence and Machine Learning technologies will further aid radiologists and clinicians across the country in accurately diagnosing diverse ailments. However, Human errors need to be guarded. A simple way to conceptualize diagnostic errors in the testing process is to classify them as preanalytical, analytic, or postanalytical [7,6].
1.Pre-analytic errors: These are the problems with test selection, ordering, & specimen collection. Such errors occur in low pretest probability of a disease, increasing the likelihood of a false positive or overdiagnosis. For example, in our reported case ultrasonography was ordered with rapid pregnancy antibody test. Underuse or overuse of diagnostic tests is frequently implicated in diagnostic error but is less often discussed in the context of diagnostic stewardship. Preanalytical errors result from specimen mishandling; or wrong person’s report getting exchanged for instance, sharing a report of someone other than the patient under test. Blood cultures are an area of special concern given high rates of use and high rates of specimen collection errors, including inadequate specimens & contamination.
2. Analytic errors: They refer to problems performing a clinical laboratory test or radiological imaging. These errors occur through inappropriate or inadequate quality control procedures, presence of substances that interfere with analysis and unskilled staff. Interpretive errors can lead to misdiagnosis as happened in our case and the second opinion reflected the actual situation. Imaging errors that occur when diagnosing a tubal pregnancy include: i) False positives- Structures, like the bowel, corpus luteum, or a Para tubal cyst, can be mistaken for an ectopic pregnancy ii) False negatives - A small ectopic pregnancy or one hidden by uterine or bowel abnormalities can go undetected on an ultrasound. iii) It can be difficult to distinguish between different types of ectopic pregnancies iv) Young Sonographers may have difficulty deciding if a gestational sac is intrauterine or ectopic.
3. Post-analytic errors: include problems with interpretation, reporting (e.g., necessary steps in the workup), and use of test results to inform diagnoses. While the failure to correctly interpret a diagnostic test result may reflect knowledge gaps or cognitive error, the problem of post analytic errors could be structure or process related.
Diagnostic imaging uses machines and techniques to create pictures of the inside of the body to help diagnose disease, plan treatment, or find out how well treatment is working. Some common imaging techniques are X-ray imaging, CT scans, MRI, and ultrasound [5].
Misinterpretation: Complex anatomy, poor lighting, and low image resolution can lead to misinterpretation of images.
Incorrect patient positioning: Incorrect positioning can lead to suboptimal images that can lead to diagnostic errors.
Failure to communicate: Inaccurate or incomplete communication of imaging results lead to diagnostic errors that are mainly process related.
Premature closure of the diagnostic process: Assigning common uncommon serious diseases (for example Tubal Pregnancy in our case report) leading to possibly fatal error or leading to unnecessary interventions and complication as was in our case.
Other types of errors include Wrong exam or wrong patient, Errors due to technical factors, and Errors due to fatigue.
In a first-trimester study of ultrasound features for diagnosis of ectopic pregnancy, an empty uterus was found to predict an ectopic pregnancy with a sensitivity of 81.1% and a specificity of 79.5%. Sensitivity and specificity for a pseudo-sac, adnexal mass, and free fluid were as follows: 5.5% and 94.2%; 63.5% and 91.4%; and 47.2% and 92.3%, respectively [8]
Challenges of Medical Imaging: Medical images contain inconsistent conditions as they are acquired under various illumination conditions and from different distances. Moreover, the images may have poor resolution, which makes the lesion detection and diagnosis difficult when it is small or in nascent stage. Perceptual errors continue to constitute the bulk of errors made and false negative errors are the frequently committed perceptual mistakes. The quality of a medical image is determined by the imaging method, the characteristics of the equipment, and the imaging variables selected by the operator, and the quality is not a single factor, but a composite of factors like contrast, blur, noise, artifacts, & distortion [5,6]
Conclusions:
Digital image processing and analysis has a critical role in clinical practice but faces Clinical, Technical, Automation, and Security Challenges.
Nearly 78% of radiologists report reading volumes beyond their capacity, which threatens patient care quality and exacerbates burnout Digital image distance measurements have two sources of error i) inherent image pixelation error and ii) modality-specific registration errors.
One of the primary challenges in medical image analysis is the scarcity of large, annotated datasets, essential for effectively training deep learning models.
Addressing this challenge requires developing techniques for efficient transfer learning and domain adaptation.
The radiologist is required to maintain the dignity of one's profession by taking a written informed consent before any investigation, explaining the examination in detail, performing the imaging in a conducive patient-friendly manner communication.
Medical Negligence happens when a healthcare provider does not meet the expected level of care, leading to injury or harm to the patient. The disputes could be a) Over Consent Validity b) Confidentiality Breaches iii) Documentation and Record-Keeping.
Unfortunately, the greater understanding of error–its frequency and to a certain extent its inevitability–which radiologists have gained over the past two decades is not shared even by colleagues in our own profession who often seem to have unrealistic expectations of the accuracy of radiological interpretation.
Consumer Redressal system in India ends with Compensation to the patients or Punitive action on the service provider in the cases of Diagnostic or Treatment errors.
Coupled with effective peer learning practices, supportive leadership, and a culture of quality, this process can unquestionably result in fewer diagnostic errors, improved patient outcomes, and increased satisfaction for all stakeholders.
Addressing this disjunction must be one of the highest current priorities for radiologists and their professional bodies
References
-
Woman wins INR 50K post misdiagnosis of Tubal Pregnancy, https://timesofindia.indiatimes.com/Mengalurru edition 16 December 2024
View at Publisher | View at Google Scholar -
Improving Diagnosis in Health Care, https://www.ncbi.nlm.nih.gov/books NBK338593
View at Publisher | View at Google Scholar -
The clinical laboratory is an integral component to health care delivery: the total testing process. Lubin IM, et al. Am J Clin Pathol 2023 Aug 1;160(2):124-129. https://doi.org/10.1093/ajcp/aqad038
View at Publisher | View at Google Scholar -
Medical Imaging Market Size, Share, & Trends 2024 to 2034, https://www.precedenceresearch.com/
View at Publisher | View at Google Scholar -
Medical Imaging in India - Recent Tech Advancements & Opportunities Ahead, https://www.siliconindia.com/41227.html
View at Publisher | View at Google Scholar -
Fundamentals of Diagnostic Error in Imaging, Jason N. Itri et.al, https://pubs.rsna.org/Doi/abs/10.1148/rg.2018180021
View at Publisher | View at Google Scholar -
Ectopic Pregnancy Ultrasound Imaging, Timothy B Jang et.al, https://emedicine.medscape.com/ 104382, 06/13/2023
View at Publisher | View at Google Scholar -
Accuracy of first trimester ultrasound features for diagnosis of tubal ectopic pregnancy: A systematic review &meta-analysis. Richardson A, et.al Ultrasound Obstet. Gynecol. 03/12/ 2015
View at Publisher | View at Google Scholar






