Case Report | DOI: https://doi.org/IJCCRI-CR-24-010.
Cutaneous Sarcoidosis Case Report
Abstract
Sarcoidosis is an inflammatory disease that affects multiple organs in the body, but mostly the lungsand lymph glands. In people with sarcoidosis, abnormal masses or nodules (called granulomas) consisting of inflamed tissues form in certain organs of the body. These granulomas may alter the normal structure and possibly the function of the affected organ(s)
Objective : to identify systemic and cutaneous disease in human body with bone marrow proliferation.
Patients and Methods : 54 years old man patient complained of fever and night sweats. He was missed diagnosed in Cairo by oncologist as diffuse large B cell lymphoma patient since 2007 due to involvement liver and lymgh nodes and he received treatment with Gemzar drug and he complete remission from liver damage . At 2015 complained of night sweats;, fever and loss of weight and high couph and reumatic pain miss diagnosed as tuberculosis T B in Jordan and he received treatment for one year without improvement. I received the patient in 2018 started appeared erythematous papulo nodular skin eruptions in his body I revised all his previous investigations . CBC , Bone marrow biopsy and aspiration, liver biopsy, hilar lymph node biopsy skin biopsy , immunohistochemical cytology zeil Nelson stain-ve ,PCR-VE, tuberclin test -ve ACE angiotenosin converting enzyme and liver function test were diagnostic plain chest xr-ay, ultrasound for liver .
Results :The clinical data and invistigations showed the pateint had non Caseating necrosis inflammatory granuloma in his thoracic lymph nodes and liver and skin most probably systemic and cutaneous sarcoidosis.
Conclusion : sarcoidosis is unknown etiology disease and treated with methotrexate and prednisolone orally with monitoring follow up..
Introduction
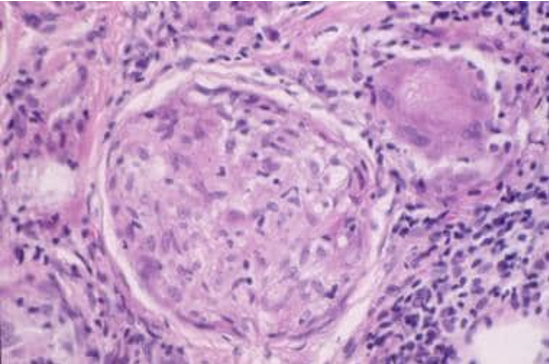
Case study 50 years old Yemeni man patient presented ill. He has fever night sweating , weight loss ,high cough and arthralgia. Plan x ray showed hilar lymphadenopathy. Abdominal ultrasonography showed hepatosplenomegaly. Bone marrow aspiration showed active proliferation and Zelnelson staining negative. Tuberculin test is negative. Skin eruptions showed fleshy papules and nodules and plaques and annular lesions in the upper back and lower limbs. ( figures 1,2,3). Skin biopsy showed hallmark noncaseating granuloma.( figure 4) The patient under treatment of methotrexate and prednisolone oral drugs. His case is stable.
Comment
Dermatologic manifestations are seen in 25% of patients with sarcoidosis. They usually accompany systemic involvement, but in some cases they may be the only manifestations of the disease. Sarcoidosis is characterized by noncaseating epithelioid granulomas that may affect any organ system. Although Jonathan Hutchinson described the first case in 1869, the etiology of the disease is still unknown. The disease most commonly involves granuloma formation in the lungs, with 90-95% of patients having some pulmonary involvement. Other commonly involved organ systems include the lymph nodes (especially the intrathoracic nodes), the skin, the eyes, the liver, the heart, and the nervous, musculoskeletal, renal, and endocrine systems. Erythema nodosum. Erythema nodosum is a hypersensitivity reaction resulting from exposure to a variety of infectious agents (especially recent streptococcal infection), drugs (including oral contraceptives), or systemic inflammatory disorders (eg, sarcoidosis, inflammatory bowel disease). EN is usually an acute, self-limiting process and rarely requires treatment. Recurrences are uncommon. Tender, erythematous nodules are usually present on the extremities, most commonly on the anterior surface of the tibia. Fever, arthralgia, and malaise may occur. EN is more common in European, especially Scandinavian, women of childbearing age than in other people. Löfgren syndrome is classically described as a triad of EN, polyarthritis, and hilar adenopathy. The adenopathy may be unilateral or bilateral hilar and/or right paratracheal lymphadenopathy. Other symptoms include anterior uveitis, fever, ankle periarthritis, arthralgias, and pulmonary involvement. Löfgren syndrome is usually an acute disease with an excellent prognosis, typically resolving spontaneously from 6-8 weeks to up to 2 years after onset. Pulmonologists, ophthalmologists, and rheumatologists often define this syndrome differently, describing varying combinations of arthritis, arthralgia, uveitis, EN, hilar adenopathy, and/or other clinical findings. Lupus pernio, first described by Besnier in 1889, is a striking manifestation of sarcoidal skin lesions. Lupus pernio is characterized by red to purple or violaceous, indurated plaques and nodules that usually affect the nose, cheeks, ears, and lips, but it can appear on the dorsa of the hands, and on the fingers, toes, and forehead. Lupus pernio is usually more common in black women with long-standing systemic, usually pulmonary, sarcoidosis than in other people. It is also commonly seen with chronic uveitis and bone cysts. The course is usually chronic, may be more recalcitrant to treatment, and may result in severe cosmetic disfigurement. Lupus pernio, especially involving the nasal rim, has been associated with granulomatous involvement of the upper respiratory tract (50%) and lungs (75%). Additionally, it is associated with a higher frequency of ocular involvement, bone cyst formation, and lymphadenopathy or organomegaly. Macular or papular sarcoidosis is the most common lesion seen in cutaneous sarcoidosis, especially in black women. Granulomatous acne rosacea may mimic sarcoidosis clinically and histopathologically. Usually, lesions are asymptomatic, red-brown macules and papules commonly involving the face, the periorbital areas, the nasolabial folds, and/or the extensor surfaces. Lesions usually resolve without scarring, although scarring may occur. These lesions may also occur in acute sarcoidosis. Periocular papules and plaques. The use of dermoscopy to aid in the clinical diagnosis of macular and plaque-type sarcoidosis has been reported, with findings of "translucent yellow to orange globular-like or structureless areas associated with linear vessels" and being associated with granulomatous skin disease, including cutaneous sarcoid. Widespread atrophic lesions with elastolysis have been reported, and widespread lichenoid lesions may resemble erythroderma. Plaque sarcoidosis is characterized by round to oval, red-brown to purple, infiltrated plaques; the center of the plaque may be atrophic. Some plaques may even appear scaly and can be confused with lesions of psoriasis or lichen planus. Dermoscopy may aid in the clinical diagnosis, as noted above. he lesions most commonly occur on the extremities, face, scalp, back, and buttocks, and they may have an annular appearance. The distribution is usually symmetrical. Angiolupoid sarcoidosis is a subtype that has a similar appearance but has large, telangiectatic vessels in addition to the characteristics mentioned above. This form of cutaneous involvement is usually chronic; most patients have the disease for more than 2 years. Lesions can heal with scarring, and, if plaques involve the scalp, they may lead to alopecia. Patients with plaque lesions usually have more severe systemic involvement. Subcutaneous nodular sarcoidosis. Subcutaneous nodular sarcoidosis is also called Darier-Roussy sarcoidosis. Lesions are usually nontender, firm, oval, flesh-colored or violaceous nodules that are 0.5-2 cm in diameter. They are commonly found on the extremities or trunk. These lesions usually appear in the beginning of the disease. Patients with these lesions often have nonsevere systemic disease. In some patients, the nodules resolve spontaneously.



References
-
Caplan A, Rosenbach M, Imadojemu S. Cutaneous Sarcoidosis. Semin Respir Crit Care Med. 2020 Oct. 41 (5):689-699.
View at Publisher | View at Google Scholar -
Caso F, Costa L, Rigante D, et al. Caveats and truths in genetic, clinical, autoimmune and autoinflammatory issues in Blau syndrome and early onset sarcoidosis. Autoimmun Rev. 2014 Aug 23. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Caso F, Galozzi P, Costa L, Sfriso P, Cantarini L, Punzi L. Autoinflammatory granulomatous diseases: from Blau syndrome and early-onset sarcoidosis to NOD2-mediated disease and Crohn's disease. RMD Open. 2015. 1 (1):e000097. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Hunt RD, Gonzalez ME, Robinson M, Meehan SA, Franks AG Jr. Ulcerative sarcoidosis. Dermatol Online J. 2012 Dec 15. 18(12):29. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Pellicano R, Tiodorovic-Zivkovic D, Gourhant JY, Catricala C, Ferrara G, Caldarola G. Dermoscopy of cutaneous sarcoidosis. Dermatology. 2010 Aug. 221(1):51-4. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Fancher W, Braniecki M, Guzman G, Groth J, Krunic A. Disseminated atrophic sarcoidosis with elastophagocytosis and elastic tissue loss. Br J Dermatol. 2014 Sep 16. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Nishizawa A, Igawa K, Teraki H, Yokozeki H. Diffuse disseminated lichenoid-type cutaneous sarcoidosis mimicking erythroderma. Int J Dermatol. 2014 Aug. 53(8):e369-70. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Jorizzo JL, Koufman JA, Thompson JN, White WL, Shar GG, Schreiner DJ. Sarcoidosis of the upper respiratory tract in patients with nasal rim lesions: a pilot study. J Am Acad Dermatol. 1990 Mar. 22(3):439-43. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Marcoval J, Maña J, Moreno A, Peyri J. Subcutaneous sarcoidosis--clinicopathological study of 10 cases. Br J Dermatol. 2005 Oct. 153(4):790-4. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Ahmed I, Harshad SR. Subcutaneous sarcoidosis: is it a specific subset of cutaneous sarcoidosis frequently associated with systemic disease?. J Am Acad Dermatol. 2006 Jan. 54(1):55-60. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Tchernev G. Cutaneous sarcoidosis: the
View at Publisher | View at Google Scholar -
Cather JC, Cohen PR. Ichthyosiform sarcoidosis. J Am Acad Dermatol. 1999 May. 40(5 Pt 2):862-5. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Antonovich DD, Callen JP. Development of sarcoidosis in cosmetic tattoos. Arch Dermatol. 2005 Jul. 141(7):869-72. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Dimitriou F, Frauchiger AL, Urosevic-Maiwald M, Naegeli MC, Goldinger SM, Barysch M, et al. Sarcoid-like reactions in patients receiving modern melanoma treatment. Melanoma Res. 2018 Jun. 28 (3):230-236. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Tchernev G, Lotti T, Wollina U, Cardoso JC, Popova LV, Maximov GK, et al. Sarcoidosis in A. C. Milan (1899)?. Open Access Maced J Med Sci. 2018 Jan 25. 6 (1):99-102. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Terziroli Beretta-Piccoli B, Mainetti C, Peeters MA, Laffitte E. Cutaneous Granulomatosis: a Comprehensive Review. Clin Rev Allergy Immunol. 2018 Feb. 54 (1):131-146. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Sibaud V. Dermatologic Reactions to Immune Checkpoint Inhibitors : Skin Toxicities and Immunotherapy. Am J Clin Dermatol. 2018 Jun. 19 (3):345-361. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Garcia-Porrua C, Gonzalez-Gay MA, Garcia-Pais MJ, Blanco R. Cutaneous vasculitis: an unusual presentation of sarcoidosis in adulthood. Scand J Rheumatol. 1998. 27(1):80-2. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Doherty CB, Rosen T. Evidence-based therapy for cutaneous sarcoidosis. Drugs. 2008. 68(10):1361-83. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Gedalia A, Molina JF, Ellis GS Jr, Galen W, Moore C, Espinoza LR. Low-dose methotrexate therapy for childhood sarcoidosis. J Pediatr. 1997 Jan. 130(1):25-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Lower EE, Baughman RP. Prolonged use of methotrexate for sarcoidosis. Arch Intern Med. 1995 Apr 24. 155(8):846-51. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Webster GF, Razsi LK, Sanchez M, Shupack JL. Weekly low-dose methotrexate therapy for cutaneous sarcoidosis. J Am Acad Dermatol. 1991 Mar. 24(3):451-4. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Jones E, Callen JP. Hydroxychloroquine is effective therapy for control of cutaneous sarcoidal granulomas. J Am Acad Dermatol. 1990 Sep. 23(3 Pt 1):487-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Baughman RP, Lower EE. Steroid-sparing alternative treatments for sarcoidosis. Clin Chest Med. 1997 Dec. 18(4):853-64. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Stagaki E, Mountford WK, Lackland DT, Judson MA. The treatment of lupus pernio: results of 116 treatment courses in 54 patients. Chest. 2009 Feb. 135(2):468-76. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Pariser RJ, Paul J, Hirano S, Torosky C, Smith M. A double-blind, randomized, placebo-controlled trial of adalimumab in the treatment of cutaneous sarcoidosis. J Am Acad Dermatol. 2013 May. 68(5):765-73. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Judson MA, Baughman RP, Costabel U, et al. Safety and efficacy of ustekinumab or golimumab in patients with chronic sarcoidosis. Eur Respir J. 2014 Jul 17. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Heidelberger V, Ingen-Housz-Oro S, Marquet A, et al. Efficacy and Tolerance of Anti-Tumor Necrosis Factor α Agents in Cutaneous Sarcoidosis: A French Study of 46 Cases. JAMA Dermatol. 2017 Jul 1. 153 (7):681-685. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Park SK, Hwang PH, Yun SK, Kim HU, Park J. Tumor Necrosis Factor Alpha Blocker-Induced Erythrodermic Sarcoidosis in with Juvenile Rheumatoid Arthritis: A Case Report and Review of the Literature. Ann Dermatol. 2017 Feb. 29 (1):74-78. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Tu J, Chan J. Cutaneous sarcoidosis and infliximab: evidence for efficacy in refractory disease. Australas J Dermatol. 2013 May 8. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Philips MA, Lynch J, Azmi FH. Ulcerative cutaneous sarcoidosis responding to adalimumab. J Am Acad Dermatol. 2005 Nov. 53(5):917. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Pariser RJ, Paul J, Hirano S, Torosky C, Smith M. A double-blind, randomized, placebo-controlled trial of adalimumab in the treatment of cutaneous sarcoidosis. J Am Acad Dermatol. 2013 May. 68(5):765-73. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Kiorpelidou D, Gaitanis G, Zioga A, Bassukas ID. Short course of infliximab for disfiguring lupus pernio. Eur J Dermatol. 2008 Nov-Dec. 18(6):727-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Kataria YP. Chlorambucil in sarcoidosis. Chest. 1980 Jul. 78(1):36-43. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Waldinger TP, Ellis CN, Quint K, Voorhees JJ. Treatment of cutaneous sarcoidosis with isotretinoin. Arch Dermatol. 1983 Dec. 119(12):1003-5. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Brechtel B, Haas N, Henz BM, Kolde G. Allopurinol: a therapeutic alternative for disseminated cutaneous sarcoidosis. Br J Dermatol. 1996 Aug. 135(2):307-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Inoue Y, Teraki Y. Association of Propionibacterium acnes with the efficacy of minocycline therapy for cutaneous sarcoidosis. Int J Dermatol. 2020 Jun. 59 (6):704-708. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Bachelez H, Senet P, Cadranel J, Kaoukhov A, Dubertret L. The use of tetracyclines for the treatment of sarcoidosis. Arch Dermatol. 2001 Jan. 137(1):69-73. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Baughman RP, Judson MA, Lower EE, Drent M, Costabel U, Flavin S, et al. Infliximab for chronic cutaneous sarcoidosis: a subset analysis from a double-blind randomized clinical trial. Sarcoidosis Vasc Diffuse Lung Dis. 2016 Jan 15. 32 (4):289-95. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Heffernan MP, Anadkat MJ. Recalcitrant cutaneous sarcoidosis responding to infliximab. Arch Dermatol. 2005 Jul. 141(7):910-1. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Carlesimo M, Giustini S, Rossi A, Bonaccorsi P, Calvieri S. Treatment of cutaneous and pulmonary sarcoidosis with thalidomide. J Am Acad Dermatol. 1995 May. 32(5 Pt 2):866-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Kalajian AH, Van Meter JR, Callen JP. Sarcoidal anemia and leukopenia treated with methotrexate and mycophenolate mofetil. Arch Dermatol. 2009 Aug. 145(8):905-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Kouba DJ, Mimouni D, Rencic A, Nousari HC. Mycophenolate mofetil may serve as a steroid-sparing agent for sarcoidosis. Br J Dermatol. 2003 Jan. 148(1):147-8. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Damsky W, Young BD, Sloan B, Miller EJ, Obando JA, King B. Treatment of Multiorgan Sarcoidosis With Tofacitinib. ACR Open Rheumatol. 2020 Feb. 2 (2):106-109. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Saylam Kurtipek G, Ataseven A, Kurtipek E, Kucukosmanoglu İ, Toksoz MR. Resolution of Cutaneous Sarcoidosis Following Topical Application of Ganoderma lucidum (Reishi Mushroom). Dermatol Ther (Heidelb). 2016 Mar. 6 (1):105-9. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Zhu X, Sun J. A case of facial atrophic sarcoidosis in an adolescent, successfully treated with the combination of prednisone and hydroxychloroquine. An Bras Dermatol. 2020 May - Jun. 95 (3):340-342. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Lee JB, Koblenzer PS. Disfiguring cutaneous manifestation of sarcoidosis treated with thalidomide: a case report. J Am Acad Dermatol. 1998 Nov. 39(5 Pt 2):835-8. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Rousseau L, Beylot-Barry M, Doutre MS, Beylot C. Cutaneous sarcoidosis successfully treated with low doses of thalidomide. Arch Dermatol. 1998 Aug. 134(8):1045-6. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Gharavi N, Diehl J, Soriano T. Cutaneous Sarcoidosis Successfully Treated With Intralesional 5-Fluorouracil. Dermatol Surg. 2015 Sep. 41 (9):1082-5. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Fazzi P. Pharmacotherapeutic management of pulmonary sarcoidosis. Am J Respir Med. 2003. 2(4):311-20. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Kaura V, Kaura SH, Kaura CS. ACE Inhibitor in the treatment of cutaneous and lymphatic sarcoidosis. Am J Clin Dermatol. 2007. 8(3):183-6. [QxMD MEDLINE Link].
View at Publisher | View at Google Scholar -
Wilsmann-Theis D, Bieber T, Novak N. Photodynamic therapy as an alternative treatment for cutaneous sarcoidosis. Dermatology
View at Publisher | View at Google Scholar






