Case Report | DOI: https://doi.org/10.5281/zenodo.17106074
Comprehensive Spine Rehabilitation Through Chakrasiddh Spine Expert Therapy (Cset): A Case of Multi-Level Musculoskeletal Disorders
Abstract
Musculoskeletal disorders affecting multiple spinal and pelvic regions can severely impair functional mobility and quality of life, especially in younger adults. This case report presents a 30-year-old female from Bangalore with a 3-year history of multi-level spinal dysfunction. She was diagnosed with Avascular Necrosis (AVN) characterized by persistent bilateral hip pain, radiating to her both limbs with left leg predominantly affected and intermittent stiffness in the upper back region, which was exacerbated during prolonged sitting or standing, significantly limiting her daily activities. The patient underwent a customized Integrative Siddha protocol, Chakrasiddh Spine Expert Therapy (CSET) for Complete spine, administered over five-weeks period, followed by scheduled follow-up evaluation after four months. The therapy is a holistic, non-invasive therapeutic approach deep rooted in siddha principles, combining targeted manual pressure manipulation techniques, postural correction, dietary alteration, and customized exercises. Pre and post therapy semi-structured interview based on scales of Visual Analogue Scale (VAS) for pain intensity, Harris Hip Score (HHS) for hip function, Oswestry Disability Index (ODI) for sciatica-related disability, and SF-36 Health Survey for overall quality of life showed substantial pain reduction, improved posture, enhanced flexibility, and restored endurance for standing and sitting.
This case highlights the potential of CSET as a comprehensive rehabilitation modality for managing multi-level musculoskeletal disorders without pharmacological or surgical intervention, offering an integrative pathway to functional recovery and improved well-being particularly in cases refractory to conventional and other alternative therapies.
Abbreviations:
CSET - Chakrasiddh Spine Expert Therapy
VAS - Visual Analogue Scale
HHS - Harris Hip Score
ODI - Oswestry Disability Index
Introduction
Musculoskeletal disorders involving multiple spinal and pelvic regions represent a significant clinical challenge due to their multifactorial etiology and the complex interplay between structural, neurological, and functional impairments. Conditions such as avascular necrosis (AVN) of the hip, sciatica, and upper thoracic stiffness are often interconnected through biomechanical chain reactions that alter posture, gait, and load distribution across the complete spine and lower limbs [1]. These disorders may result in chronic pain, reduced range of motion, impaired functional capacity, and long-term disability if left untreated or inadequately managed [2]. Although avascular necrosis (AVN) of the femoral head is reported to be five times more common in males, its occurrence in females, though less frequent, is clinically relevant. Falls, hormonal factors, Covid, metabolic disturbances such as vitamin D deficiency, autoimmune predisposition, and corticosteroid exposure may contribute to AVN risk in women [3,9]. Legg Calvé Perthes disease occurs in children where sterile necrosis of the femoral head occurs, requiring a special therapeutic approach underscoring the importance of early detection, non-invasive management, and rehabilitation strategies across age groups [4]. Present case highlights that AVN, despite its male predominance, can manifest in females due to multifactorial influences and warrants equal clinical attention. Early detection of AVN is vital for effective treatment and to minimize the progression of the disease and its associated complications. Conventional medical management for such multi-level musculoskeletal disorders often includes pain management, physical therapy, and potentially surgical interventions [3,4]. While these approaches can provide temporary symptomatic relief, they may not always address the root cause particularly the underlying biomechanical dysfunction and energy imbalance leading to frequent relapses and incomplete recovery [5]. This has given way to traditional healing systems which works on root cause and general well-being of humans.
Previous studies have evidence of Avascular necrosis manifesting symptoms beyond localized hip pain, often mimicking as sciatica and contributing to spinal stiffness and sometimes cervical pain [6]. Pain from AVN radiates to the groin, knee, anterior thigh, buttocks, and even lower back, with studies reporting referred pain in up to 77% of affected hips [6,8]. The proximity of the hip joint to the sciatic nerve makes it susceptible to referred pain patterns, where nerve irritation or compression from inflamed periarticular tissues can radiate pain down the leg, mimicking classical sciatica. This phenomenon occurs because neural and musculoskeletal pathways overlap, and hip pathology can present with pseudo-radicular symptoms, which are frequently mistaken for lumbar disc disease [7]. The intense hip pain can lead to pelvic tilt and asymmetrical load to lumbosacral spine; predisposing to disc degeneration or herniation commonly at L5-S1 levels evident as radicular pain radiating along the sciatic nerve distribution, clinically presenting as sciatica. Over time, persistent abnormal gait mechanics cause chronic overactivation of paraspinal muscles and myofascial tension, which, via the thoracolumbar fascia, propagate cranially to the thoracic and cervical regions [8]. This can lead to widespread spinal stiffness, further restricting mobility and perpetuating the pain–dysfunction cycle despite the primary lesion being localized to the hip. Central sensitization mechanisms may additionally amplify pain perception across multiple spinal levels in chronic stages. This interplay between local joint pathology, neural mechanisms, and musculoskeletal adaptation explains how AVN of the hip can manifest as a multi-regional pain and stiffness syndrome [9,10].
Siddha Medicine and CSET
Among traditional healing systems, Siddha-an ancient Indian medical practice is widely accepted by South Asian people due to its emphasis on holistic health. Beyond addressing specific diseases, this therapy is recognized for its role in maintaining overall well-being by fostering balance across the physical, mental, and emotional domains [11]. Many studies have proved Siddha to be effective way of addressing musculoskeletal diseases through individualized therapy plans and integrative approach.
Chakrasiddh Spine Expert Therapy (CSET), developed by Chakrasiddh, is an integrative Siddha-based therapy protocol designed to address complex musculoskeletal and degenerative conditions such as avascular necrosis (AVN) of the hip, chronic low back pain, and upper spinal stiffness. The therapy combines manual spinal realignment, energy channel activation, personalized yoga-based mobility regimens, and tailored dietary interventions [12]. By correcting biomechanical imbalances originating in the spine and pelvis, CSET reduces abnormal load transmission across the hip joint, thereby alleviating secondary strain on the lumbosacral and thoracic regions [9]. Targeted regimens aimed at restoring spinal alignment and improving neuromuscular control can enhance hip stability, delay degenerative progression, and mitigate referred pain patterns often mistaken for sciatica. Varmam therapy, central to CSET, involves the precise stimulation of vital energy points that regulate neuromuscular and circulatory functions. This activation restores disrupted energy flow, reduces myofascial stiffness, and improves vascular perfusion to periarticular tissues potentially benefitting patients with compromised blood supply as seen in AVN [13,14].
Complementary measures such as Siddha-based dietary regulation, simple exercise practices, and lifestyle adjustments further enhance metabolic health, reduce systemic inflammation, and promote sustained recovery [15]. The integration of dietary modifications and targeted strengthening through mobility exercises supports tissue repair, optimizes hip and spinal joint mechanics, and reduces systemic inflammation. By addressing both structural and psychosomatic contributors to pain, CSET provides a holistic approach, targeting the hip–spine syndrome where AVN-related hip pathology, abnormal gait mechanics, and compensatory thoracolumbar stiffness are interlinked [8,12]. This comprehensive framework not only relieves pain but also promotes functional restoration, psychological well-being, and a return to daily activity.
The aim of this study is to evaluate the effectiveness of Chakrasiddh Spine Expert Therapy (CSET) in improving functional outcomes, pain relief, and spinal alignment in a patient presenting with avascular necrosis (AVN) of the hip, sciatica, and upper back stiffness and improving the quality of life while potentially reducing dependence on long-term pharmacological management.
Case Presentation
A 30-year-old female from Bangalore presented with a 3-year history of bilateral hip pain, radiating pain to both lower limbs with more severity in left leg, and intermittent upper back stiffness. Symptoms worsened with prolonged sitting (>20 min) or standing (>15 min) and walking (>15 min). Functional mobility was significantly restricted, impacting both professional and personal activities. Her medical history mentioned a fall 15 years back from the chair for which she took steroids subsiding her pain gradually. The hip pain started few years back when she took a Vit B injection and gradually worsened after she had covid in 2022. Multiple consultations with orthopaedic specialists were sought, and she was prescribed non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac and aceclofenac, muscle relaxants (thiocolchicoside), and neuropathic pain modulators (pregabalin) [3,4]. Additionally, short courses of oral corticosteroids and vitamin D/calcium supplements were advised [10].
However, these measures provided only temporary or partial pain relief, with symptoms recurring within days of discontinuation. She was advised Laminectomy; to avoid surgical intervention she tried many therapies. Continuous six months of physiotherapy and trials of different alternative therapies, including ayurvedic sessions [32] and Kerala oil massages, yielded only transient symptomatic improvement, followed again by relapse of symptoms[ 5,34]. She wanted to avoid a surgery so came to Chakrasiddh for a permanent cure.
Clinical Examination [16]
On clinical examination of patient, it was noted that pain was at multiple areas. Severe pain and tenderness of Grade-3 was sensed at Bilateral hip, sacroiliac joints and lumbar region radiating towards upper thoracic region. The tenderness present at paraspinal muscles was measured at Grade-2, with stiffness at upper back region. The Positive straight leg raise (SLR) test bilaterally (suggestive of sciatic nerve irritation) was positive with left leg affected more severely as compared to right leg. On posture assessment, there was a visible mild lumbar lordosis reduction and pelvic tilt. On neurological examination of both the lower limbs' reflexes and sensations, testing was normal. Motor examination was also normal.
Diagnosis (Siddha evaluation system)
In Siddha medicine, Yugi Vaidhya Chinthamani describes Thasai Kootu Noigal (disorders of musculoskeletal origin), which bear resemblance to conditions such as avascular necrosis (AVN) and Sarakka Vaatham, where pain radiates along the course of the sciatic nerve from the lower back to the foot. According to Siddha pathology, these conditions are often associated with derangement of Vatha, leading to pain, stiffness, and restricted mobility, along with vitiation of Pittam, which contributes to inflammatory changes, localized heat, and tissue degeneration. This combined Vatha–Pittam imbalance can also manifest as upper back stiffness, muscle spasm, and nerve compression [17].
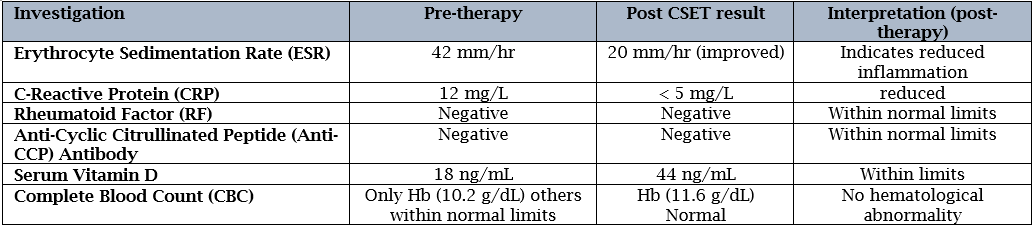
Laboratory Investigations: [16]
Relevant laboratory investigations (Table-1) were obtained to assist in accurate diagnosis and to tailor an individualized therapy protocol.
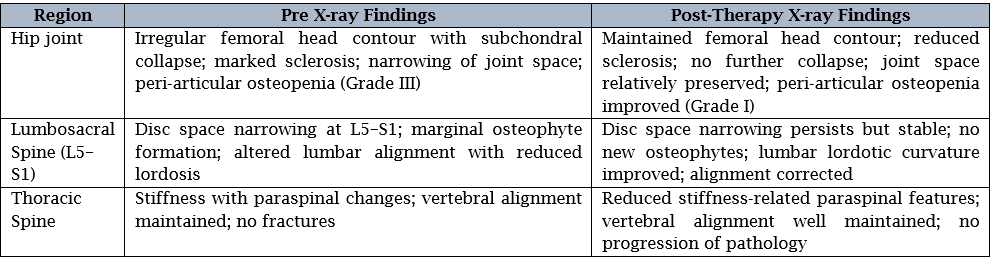
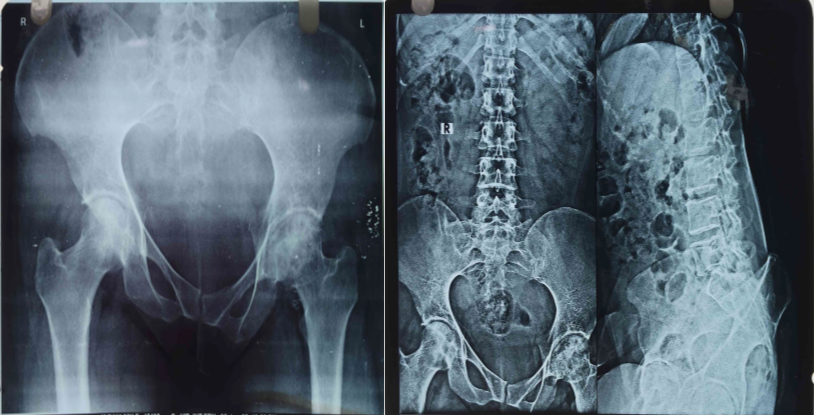
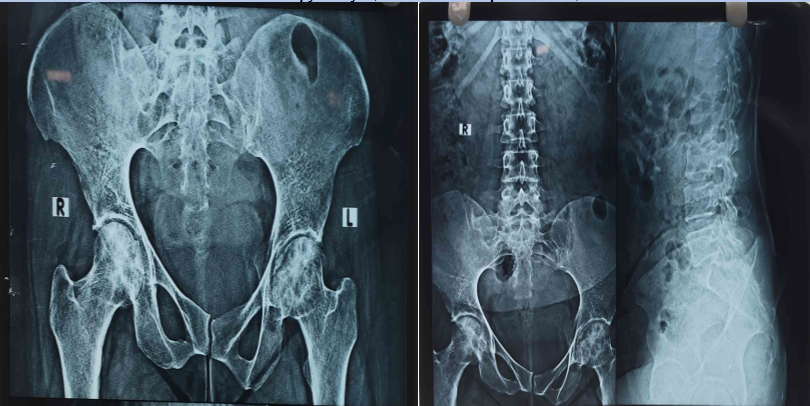
MRI and X-ray Findings:
At time of admission of patient, x-rays were taken out to compare with post therapy x-rays.
MRI Report- Lumbar spine: Early degenerative disc changes at L4–L5 and L5–S1, with mild diffuse posterior disc bulge at L4–L5 indenting the thecal sac but without significant neural compression.
Pelvis: Minimal sacroiliac joint irregularity suggestive of early sacroiliitis.
Thoracic spine: No significant disc pathology on imaging; however, clinical examination revealed upper back stiffness with paraspinal muscle spasm.
X-Ray- Avascular Necrosis, Grade III with collapse of femoral head and secondary degenerative changes (Lt hip>Rt hip). L5-S1 degenerative disc disease with foraminal narrowing, likely contributing to sciatica. Early degenerative spondylotic changes in D-3 to D-10 correlating with upper back stiffness.
Outcome Measures [6,18,19]
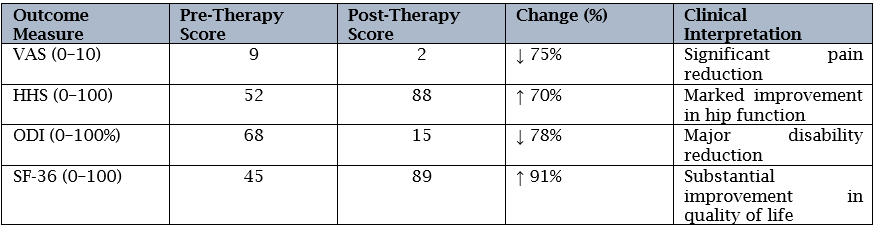
The assessment was analysed based on pre and post therapy scores of different baseline values gathered from in-house symptom tracking questionnaires and standard clinical tools built on following scales-
- VAS (Visual Analogue Scale) – Recorded pain intensity (9/10) at start of therapy
- HHS (Harris Hip Score) – Hip joint function (52/100)
- ODI (Oswestry Disability Index) – Sciatica-related disability (68%)
- SF-36 Health Survey – Quality of life (45/100)
Therapy Intervention:
The patient underwent a customized Integrative Siddha protocol, Chakrasiddh Spine Expert Therapy (CSET) for Complete spine, administered over five-weeks period, followed by scheduled follow-up evaluation after four months. CSET therapy intervention included:
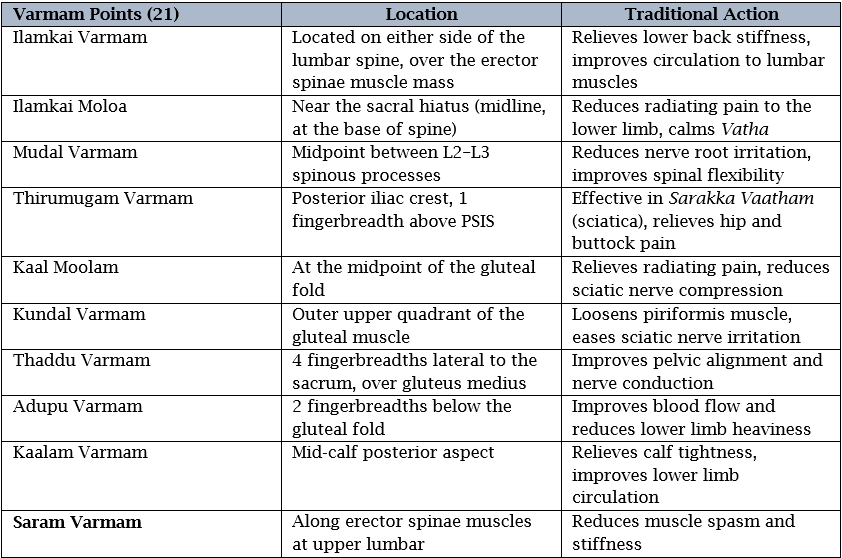
1.Targeted Manual Pressure Manipulation (Varmam & Energy points): [20-23]
This component involves applying precise, graded manual pressure to specific Varmam points as described in Siddha medicine, particularly in the lumbar, sacral, and lower limb regions relevant to AVN and sciatica for 30-40 minutes daily for 22 days (Table-2). The stimulation helps release muscle tension, reduce nerve compression, improve blood flow, and restore the balanced flow of Vatha energy. Integrated energy therapy techniques—gentle touch, rhythmic breathing, and focused intention—are used to harmonize bio-energetic pathways (nadis), supporting inflammation control and tissue healing.
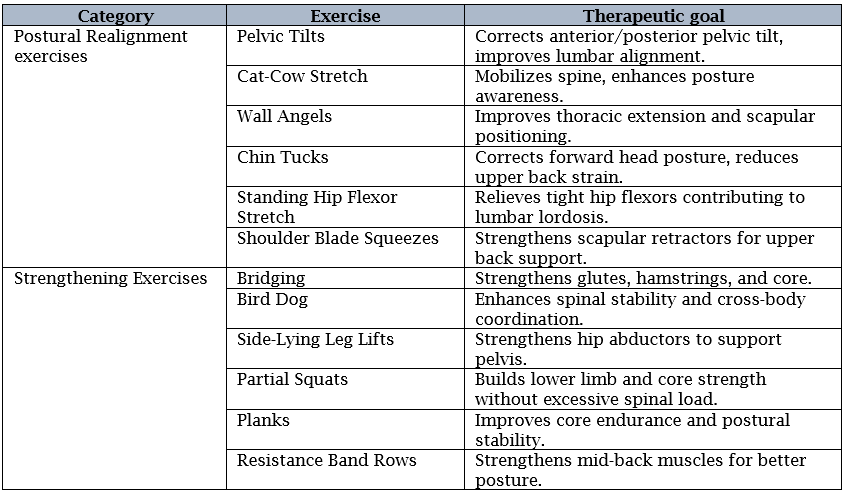
2. Postural Realignment and Strengthening exercises: [19]
To correct spinal curvature, pelvic tilt, and gait imbalances along with strengthening core, hip, and back muscles, individualized exercise program was designed. The exercises were performed for 10 minutes daily (Table-3)
3. Siddha-Based Dietary Modifications: [24]
Dietary guidance follows Siddha principles for pacifying aggravated Vatha and Pittam, focusing on warm, easily digestible, anti-inflammatory foods. Spices such as turmeric, dry ginger, and cumin are incorporated for their Vatha-balancing and circulation-enhancing properties, while cold, dry, and excessively spicy foods are avoided. Adequate hydration and seasonal adjustments are emphasized to support joint lubrication and metabolic stability.
Results
The pre- and post-therapy evaluation using validated clinical scales provides an objective measure of the patient’s progress under CSET intervention. Post-CSET, the VAS score showed a significant reduction (VAS ↓ 75%), indicating effective pain relief and improved comfort during daily activities. The improved HHS score (HHS ↑ 70%) reflected enhanced hip mobility, reduced limp, and greater ease in performing functional tasks such as sitting, standing, and walking endurance.
The Oswestry Disability Index (ODI) score measuring disability related to lower back pain was very high pre-CSET (68). After CSET therapy, the marked reduction in ODI score (15) demonstrated ODI reduced 78%, enhancing spinal function and reduced disability. The SF-36 Health Survey evaluates overall quality of life across eight domains, including physical functioning, bodily pain, vitality, and social functioning. Initially, poor scores in multiple domains reflected pain-related physical and emotional distress. Post-therapy, the rise in SF-36 scores (89/100) indicated better general health perception, greater activity tolerance, and improved psychosocial well-being (SF-36 ↑ 91%). Collectively, these improvements validate the multi-dimensional benefits of CSET in this case. (Table-4)
On re-examination following therapy, the patient showed marked clinical improvement. Pain intensity had reduced considerably, with only mild intermittent discomfort reported at the bilateral hip and lumbar region. Tenderness decreased from Grade-3 to Grade-1 at the hip, sacroiliac joints, and lumbar spine, and was absent in the thoracic region. Paraspinal muscle tenderness was minimal (Grade-0 to Grade-1), and upper back stiffness had largely resolved. The Straight Leg Raise (SLR) test was negative bilaterally, indicating relief from sciatic nerve irritation. Postural assessment revealed restoration of lumbar lordosis and correction of the previously observed pelvic tilt. The elevated levels of ESR and CRP had reduced and were in normal ranges and levels of Hb raised from 10.2 g/dL to 11.6 g/dL. The post therapy radiographic findings clearly depicted reduced sclerosis, lumbar curvature improvement and reduced stiffness (Table-5)
Following the completion of CSET, the patient experienced a marked improvement in functional endurance, being able to sit comfortably for over two hours and stand for up to one hour without significant discomfort. She was able to resume prolonged computer work, household chores, and social activities that had previously been limited by pain. At the 4-month follow-up, these functional gains were maintained, with no relapse of symptoms, indicating sustained benefit in daily living performance.
Discussion:
Musculoskeletal disorders sometimes involve multiple spinal regions and present a significant clinical challenge due to their multifactorial etiology and the complex interplay between structural, neurological, and functional impairments [6]. Though, more common in males, this case attracted the attention being present in a female patient; due to multifactorial influences and warrants equal clinical attention [3]. Like in this case, the patient had a fall and the case worsened after covid which is found in many recent studies [9]. Such cases require an integrative approach of multiple therapies along with conventional management [5]. While these approaches may provide symptomatic relief, they often fail to address the complex interplay between musculoskeletal, neural, and systemic factors contributing to disease progression.
This case illustrates that CSET can be effective in multi-level spinal disorders, even in chronic and refractory cases and compared to conventional methods, CSET provided not only symptom relief but also functional restoration. The application of CSET in this case of bilateral hip pain due to early-stage avascular necrosis (AVN), sciatica, and upper back stiffness; conditions that are often characterized by significant pain, restricted mobility, and progressive functional impairment, the post-therapy results indicated positive results in presenting enhanced hip mobility, reduced limp, and greater ease in performing functional tasks such as sitting, standing, and walking endurance as shown by other studies in which VAS, and quality of life improved [12,22]. The combination of manual pressure techniques, posture correction, and lifestyle-based interventions likely contributed to biomechanical realignment and neuromuscular rehab.
CSET moduled by Chakrasiddh, offers a distinct model by integrating Siddha principles of disease causation with targeted biomechanical and neurovascular interventions. In Siddha medicine, Yugi Vaidhya Chinthamani describes Thasai Kootu Noigal (musculoskeletal disorders) and Sarakka Vaatham (sciatic nerve pain), attributing their origin to derangement of Vatha and Pittam. In AVN and sciatica, Vatha derangement is thought to impair structural integrity and nerve conduction, while Pittam aggravation contributes to inflammation and tissue degeneration. In upper back stiffness, Vatha imbalance manifests as muscle rigidity and restricted spinal movement, compounded by Pittam-mediated inflammatory processes [17]. CSET addresses these disruptions by combining spine realignment techniques, varmam (vital energy point) stimulation, and individualized dietary and lifestyle modifications including mild exercises and yoga to restore systemic equilibrium. In this case, action was directed not merely at the site of pain but also at correcting postural imbalances, reducing nerve compression, improving circulation, and calming Vatha-Pittam disturbances. The clinical outcome measured on VAS, HHS and ODI scales presented sustained pain reduction, improved mobility, and enhanced quality of life measured without pharmacological dependence as already achieved in previous case reports of AVN patient [22,26].
CSET’s multimodal approach aligns with the principles demonstrated in recent Siddha research. For instance, in a randomized controlled trial on plantar fasciitis, it was reported that Varmam therapy combined with energy sessions resulted in superior pain relief and functional improvement compared to NSAIDs, with sustained benefits and no relapse during follow-up [27]. This mirrors the current case, where the patient experienced lasting relief in pain and improved sitting/standing tolerance without recurrence at four months follow-up. Similarly, another single case documented of lower back pain mentioned Varmam therapy significantly reducing joint pain and decreased reliance on pharmacological interventions [24]. The observed systemic impact on inflammatory symptoms supports the premise that manual pressure on key energy points can influence both local musculoskeletal pathology and broader neuroimmune responses, as seen in the present case. In another clinical study conducted at the Government Siddha Medical College, Chennai, on Vatha disorders found significant improvement in pain scores and mobility in patients with lumbar spondylosis using varmam therapy combined with herbal medicines [28]. Another study on Periarthritis reported reduction in joint swelling and pain after Siddha herbal-mineral formulations and external therapies [29]. Research on varmam point stimulation has demonstrated measurable increases in peripheral circulation and reductions in muscle spasm, suggesting plausible mechanisms for its benefits in sciatica and back stiffness [30]. A report on lumbar degenerative Spondylolisthesis showed positive results on application of both Siddha Marma (Energy) and Thokkanam therapy for 22 days in terms of flexibility and mobility in the joint area [31].
When compared to other alternative therapies, CSET shows lot of similarity to the process that are followed by them like Ayurveda employs therapies such as Panchakarma (detoxification), medicated oil massages (Abhyanga), and herbal formulations for AVN and sciatica which aligns with varmam point manipulations in siddha [32]. Naturopathy focuses on diet, hydrotherapy, and yoga-based rehabilitation, which can improve general health and musculoskeletal function, but may lack the targeted neuromechanical corrections central to CSET [33]. Chiropractic and osteopathic manipulations in Western alternative medicine offer structural realignment benefits but typically do not integrate systemic energetic balancing, a key component of Siddha-based care [34]. The therapeutic principles demonstrated in multiple physiotherapy and mobility exercise studies closely align with the clinical approach of Chakrasiddh Spine Expert Therapy (CSET). Evidence from randomized controlled trials and meta-analyses confirms that structured, stabilization-focused exercises—such as core strengthening, yoga, and tai chi—can significantly reduce pain and improve functional mobility in patients with chronic low back pain. These modalities emphasize key biomechanical objectives like postural correction, spinal realignment, and core activation, which are central to the framework of Chakrasiddh Spine Expert Therapy (CSET) [35,36]. Evidence from energy-touch modalities such as Reiki demonstrates reductions in pain and anxiety versus control/sham in pooled analyses, with one lumbar-pain trial reporting outcomes comparable to physiotherapy, though overall certainty remains limited by small samples and risk of bias [37].
Our CSET protocol integrates these themes (targeted energy point stimulation, and structural realignment) and produced concordant gains across VAS, ODI, HHS, and SF-36. Although formal scientific research on Siddha interventions is still emerging, several studies have reported positive outcomes in chronic musculoskeletal conditions. While these studies are often small-scale and lack the methodological rigor of randomized controlled trials, they provide preliminary support for the musculoskeletal benefits of Siddha-based approaches.
Conclusion
This case-based exploration highlights the therapeutic potential of Chakrasiddh Spine Expert Therapy (CSET) and targeted pressure point interventions in managing complex musculoskeletal and neurogenic conditions, such as avascular necrosis (AVN), sciatica, and upper back stiffness. The therapy presents a promising, non-invasive, and holistic approach for the comprehensive rehabilitation of complex musculoskeletal disorders, especially in younger adults where pharmacological and surgical options are not preferred. While conventional pharmacological and physical therapy approaches often provide only temporary symptomatic relief, the observed outcomes in this case suggest that addressing the underlying Vatha and Pittam disruptions—along with structural alignment and muscular balance—may facilitate sustained improvement in pain, mobility, and overall functional capacity. Although these encouraging results are drawn from a single case, larger, well-designed clinical trials are warranted to scientifically validate the safety, reproducibility, and long-term efficacy of CSET in degenerative and nerve-compression–related disorders. Such evidence could position Siddha-based interventions as valuable complementary options within an integrative musculoskeletal care framework.
References
-
Lewis CL, Sahrmann SA. (2015) Effect of posture on hip angles and moments during gait. Man Ther.;20(1):176-182. doi:10.1016/j.math.2014.08.007.
View at Publisher | View at Google Scholar -
Shah KN, Racine J, Jones LC, Aaron RK. Pathophysiology and risk factors for osteonecrosis. Curr Rev Musculoskelet Med. 2015;8(3):201-9. doi:10.1007/s12178-015-9277-y.
View at Publisher | View at Google Scholar -
Wu T, Jiang Y, Tian H, Shi W, Wang Y, Li T. Systematic analysis of hip-preserving treatment for early osteonecrosis of the femoral head from the perspective of bibliometrics (2010–2023). J Orthop Surg Res. 2023;18(1):959. doi:10.1186/s13018-023-04435-8.
View at Publisher | View at Google Scholar -
Rodríguez-Olivas AO, Hernández-Zamora E, Reyes-Maldonado E. Legg-Calvé-Perthes disease overview. Orphanet J Rare Dis. 2022;17(1):125. doi:10.1186/s13023-022-02275-z
View at Publisher | View at Google Scholar -
Sai Krishna MLV, Kar S, Kumar R, Singh H, Mittal R, Digge VK. The role of conservative management in avascular necrosis of the femoral head: a review of systematic reviews. Indian J Orthop. 2023;57(3):410-20. doi:10.1007/s43465-023-00818-5.
View at Publisher | View at Google Scholar -
Lee YK, Ha YC, Cho YJ, Suh KT, Kim SY, Won SH, et al. Referred pain to the buttock, thigh, and leg from avascular necrosis of the femoral head. Clin Orthop Relat Res. 2012;470(6):1592-8. doi:10.1007/s11999-011-2185-7.
View at Publisher | View at Google Scholar -
Santillán DM, Hyun JS, Osuna CJC, et al. Hip-spine syndrome: A challenge in its diagnosis and treatment. Cir Columna. 2024;2(4):237-46. doi:10.35366/118097.
View at Publisher | View at Google Scholar -
Prather H, van Dillen L. Links between the hip and the lumbar spine (hip spine syndrome) as they relate to clinical decision making for patients with lumbopelvic pain. PM R. 2019;11(S1):S64-S72. doi:10.1002/pmrj.12187.
View at Publisher | View at Google Scholar -
Avascular necrosis as a part of ‘long COVID-19.’” BMJ Case Rep. 2021;14(7):e242101. doi:10.1136/bcr-2021-242101.
View at Publisher | View at Google Scholar -
Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, MRI, MRA, and intra-articular injection in hip disorders. Am J Sports Med. 2004;32(7):1668-74. doi:10.1177/0363546503262201.
View at Publisher | View at Google Scholar -
Kalaiarasi C, Priya DK, Muthukumar NJ. A cross-sectional study on varmam practice by traditional practitioners & Siddha physicians in the management of pakkavatham and mugavatham. Int J Creative Res Thoughts. 2022;10(12):1880-90.
View at Publisher | View at Google Scholar -
Sathya SB, Sankar I, Shweta T. Holistic management of chronic low back pain and ACL tear using Chakrasiddh Spine Expert Therapy (CSET): a case report. Open Access J Med Healthc. 2025;1(2):1-8.
View at Publisher | View at Google Scholar -
Dharshini P, Mozhi PA, Sundaram MM, VB. The efficacy of Siddha medicine Braminei with varma therapy in manthasanni (autism spectrum disorder) in children: a case report. Int J Ayurveda Pharma Res. 2018;6(5).
View at Publisher | View at Google Scholar -
Sindhuja G, Subramanian N, Kannan M, et al. Clinical evaluation of Siddha Varmam therapy in lumbar disc prolapse (Thandagavadham). J Res Siddha Med. 2018;1(1):1-8.
View at Publisher | View at Google Scholar -
Sindhuja BS, Sankar I, Tiwari S. Siddha approach in rehabilitation of a patient with foot drop using Chakrasiddh Spine Expert Therapy (CSET): a case report. J Neurol Neurosurg. 2025;1(1):1-6.
View at Publisher | View at Google Scholar -
Lee WQ, Lie HM, Lie DTT. Diagnosis and treatment of avascular necrosis of the humeral head: current concepts. J ISAKOS. 2023;8(2):108-13. doi:10.1016/j.jisako.2022.11.002.
View at Publisher | View at Google Scholar -
Thas JJ, Balachandran P, Srinivasan S, Senthilnathan R. Effect of Varmam therapy on Santhu Vatham (knee osteoarthritis): a single patient study. Int J Pharm Pharm Sci. 2017;9(7):262-5. Available from: https://journals.innovareacademics.in/index.php/ijpps/article/view/20487.
View at Publisher | View at Google Scholar -
Lewis R, Williams N, Matar HE, Din N, Fitzsimmons D, Philips C, et al. The clinical effectiveness and cost-effectiveness of management strategies for sciatica: systematic review and economic model. Health Technol Assess. 2011;15(39):1-484. doi:10.3310/hta15390.
View at Publisher | View at Google Scholar -
Hansson EE, Stålnacke BM, Stjernberg L, et al. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976). 1996;21(14):1648-53. doi:10.1097/00007632-199607150-00013.
View at Publisher | View at Google Scholar -
Ramya V, et al. Validation of varma points for thandagavatham—a case series. J Res Biomed Sci. 2020;3(2):48-51.
View at Publisher | View at Google Scholar -
Kavitha K, Bhagyalakshmi B, Ramya V, Samundeswari P, Muthukumar NJ, Mahalakshmi V. Effectiveness of Varmam therapy and Kombarakku Ottradam in lumbar retrolisthesis: a case report. J Nat Remedies. 2024;24(5).
View at Publisher | View at Google Scholar -
Sindhuja BS, Sankar I, Reddy RM, Tiwari S. Conservative management of avascular necrosis by Siddha therapy without medicines and surgical intervention: a case study. Int J Sci Res. 2023;12(10):1507-10. doi:10.21275/SR231019205047.
View at Publisher | View at Google Scholar -
Sindhuja G, Kannan M, Manoharan N, et al. Efficacy of Varmam therapy in lumbar disc herniation: a clinical study. Int J Ayurveda Pharma Res. 2019;7(9):1-6.
View at Publisher | View at Google Scholar -
Sindhuja G, Kannan M, Subramanian N, et al. Role of Siddha Varmam in reducing low back pain and improving functional mobility in disc prolapse: a comparative study. Int J Res Pharm Sci. 2020;11(3):400-6.
View at Publisher | View at Google Scholar -
Aishwarya A, Kantham TL, Meenakumari R. Siddha dietary and lifestyle pattern: a shield to win the COVID-19 pandemic battle. Int J Herb Med. 2020;8(6):19-27.
View at Publisher | View at Google Scholar -
Duraipandiyan V, Alagappan M, Balu S. Dosha: the basic concept in Siddha therapy. Int J Res Pharm Sci. 2019;10:365-70.
View at Publisher | View at Google Scholar -
Sindhuja G, et al. Comparative study of managing plantar fasciitis by integrated Siddha varmam and energy healing vs conservative treatment. Curr Sci Res Biomed Sci. 2024;5(1):180027.
View at Publisher | View at Google Scholar -
Sindhuja G, Kannan M, et al. Varmam therapy combined with Thokkanam in lumbar spondylosis: an interventional study. Int J Res Ayurveda Pharm. 2021;12(6):25-31.
View at Publisher | View at Google Scholar -
Lakshmi T, Mohan R, Vijayalakshmi R. Efficacy of Varmam therapy with Ottradam in Kumbavatham (periarthritis): a case report. Int J Health Sci Res. 2025;15(4):106-10. Available from: https://www.ijhsr.org/IJHSR_Vol.15_Issue.4_April2025/IJHSR-Abstract14.html.
View at Publisher | View at Google Scholar -
Priya BK, Aishwarya A. Effectiveness of Siddha purgative therapy and varmam in thandagavatham (lumbar spondylosis) and sciatica. J Global Biosci. 2021;10(3):8417-29.
View at Publisher | View at Google Scholar -
Sindhuja BS, Sankar I, Tiwari S. Management of lumbar degenerative spondylolisthesis by Siddha Marma (energy) and Thokkanam therapy: a case report. Int J Clin Case Rep Rev. 2025;23(3). doi:10.31579/2690-4861/703.
View at Publisher | View at Google Scholar -
Sharma A, Sharma S, Sharma R. Ayurvedic management of Gridhrasi (sciatica): a clinical review. J Ayurveda Integr Med. 2020;11(4):563-70. doi:10.1016/j.jaim.2018.05.006.
View at Publisher | View at Google Scholar -
Arankalle DV. Integrating naturopathy and yoga in management of musculoskeletal disorders. Int J Prev Med. 2013;4(1):120-1. PMID:23413399.
View at Publisher | View at Google Scholar -
Vickers A, Zollman C. ABC of complementary medicine. The manipulative therapies: osteopathy and chiropractic. BMJ. 1999;319(7218):1176-9. doi:10.1136/bmj.319.7218.1176.
View at Publisher | View at Google Scholar -
Zhu F, Zhang M, Wang D, et al. Yoga vs non-exercise or physiotherapy exercise on pain, disability, and QoL in chronic low back pain: a systematic review. PLoS One. 2020;15(9):e0238544. doi:10.1371/journal.pone.0238544.
View at Publisher | View at Google Scholar -
Luomajoki H, et al. Core stability exercise vs general exercise for chronic low back pain: a meta-analysis. Eur Spine J. 2012;21(11):2189-97. doi:10.1007/s00586-012-2319-6.
View at Publisher | View at Google Scholar -
Kumar S, Bhatia R, Kaur M. Effect of Reiki therapy on pain, anxiety and QoL in patients with chronic low back pain: a randomized controlled trial. Complement Ther Clin Pract. 2021;42:101295. doi:10.1016/j.ctcp.2020.101295.
View at Publisher | View at Google Scholar






