Research Article | DOI: https://doi.org/IJCCRI/RW/007
Clinical Evaluation of Class II Restorations Using UniversalAdhesive;3 Years
Abstract
The purpose of this study; To retrospectively evaluate the 3-year clinical performance of class II restorations using six different composite restorative materials together with universal adhesives in patients treated. From the voluntary patient group, which included 186 restorations in a total of 105 patients included in the study, 85 patients agreed to come for a control 3 years after the date of procedure, and a total of 141 restorations were evaluated by an only one dentistaccording to modified USPHS criteria. According to the criteria evaluated in our study, the success rate of dental composite materials was determined as 98.6%. Therewas no statistically significant difference in clinical success between all dental composite material groups (p>0.05). All dental composite materials used in the study showed clinically acceptable success rates of over 90% as a result of a 3-year retrospective evaluation.
Abbreviations
% Percent
nm nanometer
μm micrometer
A Alfa
B Bravo
C Charlie
UDMA urethane dimethacrylate
USPHS United States Public Health Service
Introduction
Dental composite materials are Bis GMA based resins introduced in the early 1960s.1 This material, which literally means complex materials, consists of synthetic polymers, fillers, dimethacrylate monomers, cross-linked polymers, molecules that initiate the polymerization reaction, inhibitors, pigments and silane coupling agents.2,3 Dental composite materials typically consist of three chemical constituents: organic matrix, inorganic matrix, and intercalating agent.4 The inorganic matrix increases the strength of the restorative material and improves the physical properties of the composite by reducing thermal expansion. In order to increase the mechanical properties of the composite material and reduce its solubility and water absorption, the intercalating agent should provide a strong bond between the organic matrix and the inorganic matrix.3 In current composite resins, the organic matrix structure consists of monomers, co-monomers, inhibitors, polymerization initiators and ultraviolet stabilizers to provide the material with optimum optical, mechanical and clinical properties.5, 6 Chewing forces, occlusal habits, abrasive foods and liquids, temperature and humidity changes, bacterial by-products and salivary enzymes affect the life of composite restorations.7 However, results from long-term clinical studies demonstrate the long-lasting success of composite restorations when placed correctly.2Modifications to composite resins improve their physical and mechanical properties. Various shades, transluce, effects and opacities allow today's composites to mimic the optical properties of natural teeth.4
Dental composite material classification is as shown Table 1.1.8,9
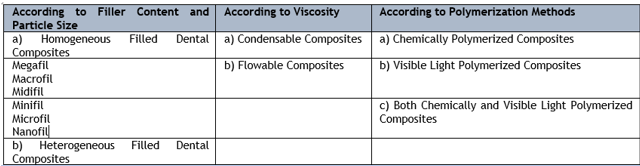
Composites are commonly divided into three groups according to filler size and inorganic filler distribution; traditional, microfilled and hybrid composites.3,10 Traditional composites (macrofil) contain 75-80% by weight and 50-60% by volume inorganic filler.10 The relatively large size of the filler particles results in the abrasion of the material and the deterioration of its surface properties. To solve this surface irregularity problem seen in traditional composites, dental composite materials with smaller filler sizes have been developed. Microfill composites with an average fillersize of 0.01-0.04 μm allow a smoother and more polished surface to be finished. They have an inorganicfiller content of 35-60% by weight and have lower physical and mechanical properties than traditional composites. Clinically resistant to abrasion, microfill composites allow restorations to flex with the tooth with their low elasticity modules. Hybrid composites have been developed by combining the positive physicaland mechanical properties of macrofill composites with the typical polishable properties of microfillcomposites. They contain 75-85% inorganic filler by weight.11 These composites, whose particle size is smaller than macro-filled compositesand whose particle amount is greater than micro-filled composites, are named according to the large particle size.6 They can be used on both front and back teeth. 4 With recent developments in dental composites, composites containing only nanoscale fillers have begun to be developed. Nanofilled composites contain more nanoparticles and prepolymerized resinfillers as in microfilled composites, in addition to the hybrid composite formulation.12 Thus, polymerization shrinkage is reduced and mechanical, optical and polishable properties are increased.6 During the polymerization reaction, the monomers in the organic matrix become polymersand shrink in
volume. There is no change in the inorganicphase. Therefore, when the ratio of inorganic fillersin the structure of composite resins is increased, the amount of polymerization shrinkage will also decrease.13 The incorporation of small fillers such as nanofilled silica particles into the structure of composite resins greatly reduced polymerization shrinkage and stresses in microfilled and hybrid composites.6
In vitro studies are carried out to evaluate the biocompatibility of the materials used on tissues and to predictpossible possibilities.14 The fact that the experimental environment is controllable, cheap, easy and repeatable provides insight into problems that may arise in in vivo studies.15 Prospective or retrospective in vivo studies are performed to monitor the clinical performance of restorative treatments. In the evaluation of these clinical studies, modified USPHS criteria, modified Ryge criteria and FDI criteria with units ranging from excellent to poor can be used.16
The purposeof this study was to:
- Determine the clinical performance of posterior composite restorations using modified USPHS criteria,
- Examine the clinical survival rates of posterior composite restorations over time.
Materials Methods
Our study includes patientsbetween the ages of 18- 25, with acceptable oral hygiene, without any pulpal or periodontal disease symptoms and systemic health problems, and who applied to the restorative dental treatment clinic due to caries. Patients who had any systemic health problems, had deep class II restorations, refused to participate in the study, and were unable to attend follow-up controls were excluded from the evaluation. The power analysis of this studywas
performed with the statistical power calculation program (G-Power, ver. 3.1.9.4 F.Paul, Kiel University, Germany) and a total of 141 restorations were included in the study, with a minimum of 15 restorations in each group. The standard procedure followed for restoration construction is;
- Preparation of the cavity should be done with medium-sized green belt diamond roulette bur under water cooling system using high-speed motors,
- Cleaning the carieswith tungsten carbidebur after reaching the dentin tissues,
- Isolating the operation area with cotton pads in addition to saliva ejector systems after the caries is completely removed,
- Limiting the restoration area with matrix tape (Super MattTM Adapt SuperCap Matrix, Kerr, Switzerland or Quickmat DELUXE, Polydentia, Switzerland,) and wedge,
- Applying the universal adhesive system to the cavity with micro brushes according to the
manufacturer's instructions,
- Ensuring polymerization using VALO Cordless (Ultradent, South Jordan, UT, USA) light device,
- Placing the selected composite material into the cavity using the layering method with a maximum thickness of 2 mm with the help of hand tools,
- Lighting each layer from all directions for 20 s,
- After the procedure is completed, articulation paper (RAYDEN INC, North Carolina, USA),
- Correction of the excess with yellow belt diamond finishing burs (60 and 40 m grit) and polishing (Shofu one gloss, Shofu Co, Japan),
- Removal of the oxygen inhibition layer on the interproximal surfaces of all restorations with aluminum oxide belt sanders(ZENIT flex, President Dental, Germany),was determined as follows.
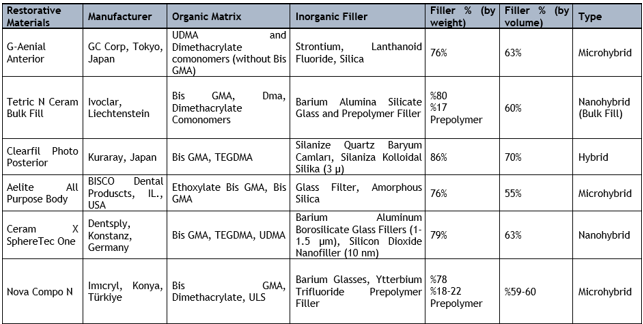
The date of the restorations made with the described procedures (Table 2.1), the adhesive resin and restorative material used during the making were recorded and follow-up groups were created.
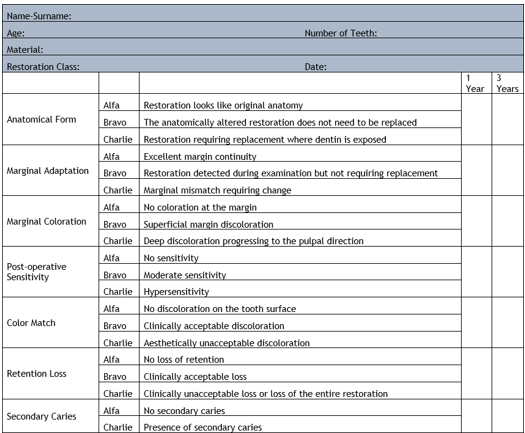
A total of 105 patients were included in these groups. Three years later, the tooth and restoration surfaces of the patients included in the follow-up process were evaluated according to the Modified USPHS criteria. According to these criteria; stability of the anatomical form, marginal adaptation changes and possible marginal discolorations, whether the patient developed any sensitivity after the procedure, tooth and restoration color harmony, presence of retention areas and secondary caries supported by radiographs were evaluated. The scores of the findings were grouped as follows;
- Alpha (A), clinically excellent success
- Bravo (B), clinically acceptable success
- Charlie (C), clinically unacceptable success17
All data collected were recorded on the evaluation form together with the dental photographs taken. (Table 2.2)
Each of the ModifiedUSPHS criterion data obtained from volunteer patientswhose teeth were restored using different dental composite materials and included in the study were statistically evaluated in pairs using the Two Proportion Test.
Results
Of the volunteer group consisting of 67 female(112 restorations) and 38 male (74 restorations) patients with completed restorations, 54 female (92 restorations) and 31 male (49 restorations) patients agreed to participate in this retrospective study. All patients were interviewed by phone for a 3-year evaluation and were recalled to the clinic. Unfortunately, 15 of the patients could not be reached, and 1 patient in the Nova Compo N patient group was removed from the study group because his restoration was changed due to secondary caries after 1 year. In this study conductedon volunteer patients, 81% (85 patients) of 186 Class II restorations of 105 patients were reached after 3 years, and 75.8% (141 restorations) of the restorations were re-examined. In the G-aenial Anterior Composite group, 73%, in the Tetric N Ceram Bulk Fill group, 72%, in the Clearfil Photo Posteriorgroup, 60%, in the Aelite All PurposeBody group, 86%, in the CeramX SphereTec One group, and 94% in the Nova Compo N group, re- examination was performed. 141 restorations were evaluated according to the modified USPHS criteria. The number and percentage distribution of the scores obtained by retrospective evaluation of restorations made using differentdental composite materials after 3 years are shown in Table 3.1.
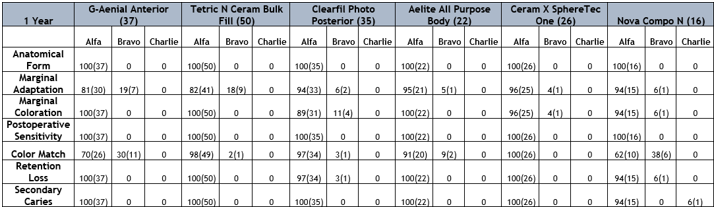
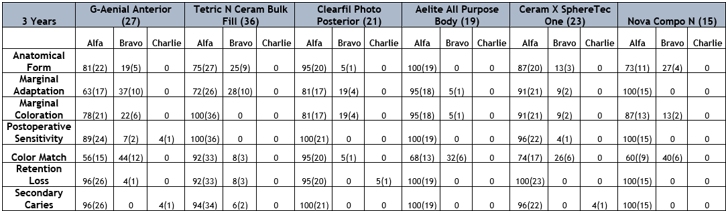
When the restorations in our study were evaluated according to the modified USPHS Criteria; in the anatomical form examination, the clinically acceptable B score was seen more in the G-Aenial Anterior Composite group among five different dental composite materials. In the Aelite All Purpose Body group, all restorations were recorded as Ascore. In the marginal adaptation evaluations, the highest B score was seen in the G-Aenial Anterior Composite and Tetric N Ceram Bulk Fill groups. All restorations in the Nova Compo N group were recorded as A score. The highest B score for marginal discoloration value was seen in the G- aenial Anterior Composite and Clearfil Photo Posterior groups,while the Tetric N Ceram Bulk Fill group received the highest A score. The only C score for postoperative sensitivity was detected in the G-aenial Anterior Composite group, and there was no difference between the Tetric N Ceram Bulk Fill, Clearfil Photo Posterior, Aelite All Purpose Body and Nova Compo N groups, and A score was recorded in all restorations. In the color match evaluation, the highest B scores were detected in the G-aenial Anterior Composite and Nova Compo N groups. For retention loss, C score was recorded only in one restoration in the Clearfil Photo Posterior group. There was no difference between the Aelite All PurposeBody, CeramX Spheretec One and Nova Compo N groups, and all restorations were recorded as A score. In the secondary caries evaluations, C score was recorded in the G-aenial Anterior Composite and Ceramx Spheretec One groups. There was no difference between the Clearfil Photo Posterior, Aelite All Purpose Body and Nova Compo N groups, and all were recorded as A score.
Discussion
The overall clinical success of dental composites is multifactorial, therefore a series of in vitro and in vivo studies are needed.18 The results obtained from in vitro studies are informative about the clinical performance of the dental composite materials used.19 With the in vivo studies and standard evaluations, the healthiest possible restorations are made in the patient's mouth.20
Clinical follow-up is required at certain periods to evaluate the success of the materials used and the restorations made in dentistry.21 Studies indicate that the long-term performance of materials will deteriorate over time at marginaledges, regardless of the placement technique.19 In addition to the fact that the long-lasting clinical success of restorations made with dentalcomposite materials in both the anteriorand posterior regionsis related to various factors related to the operator and the material, the most important factors to be considered are appropriate placement techniques and the optimum level of polymerization. It has been stated that the successrate of materials with improved mechanical and physical properties will increase.22 In accordance with the changing conditions in the oral environment, the properties of dental composite materials such as thermal expansion coefficient, elastic modulus and water absorption should exhibit similar behavior. Hybrid composites with increased inorganic filler ratio that meet these conditions are preferred in posteriorrestorations.21 Standard programssuch as the USPHS criteria and the ADA acceptance program continue to be used today for routine clinical evaluations. However, "modified USPHS criteria" have been developed that include additional parameters such as postoperative sensitivity and surface properties.17
Studies have shown that the location of the restoration plays a role in the formation of secondary caries. It has been found that under optimum oral hygiene, cervical composite restorations (class V) are the least affected by secondary caries, while the highest incidence of secondary caries is in class I and class II restorations made in the posterior region.23 In our study where we used modified USPHS evaluation criteria, in restorations made in class II cavities, the secondary caries formation percentage was determined as 4% in two dental composite materials (G-aenial Anterior composite and CeramX SphereTecOne) at the end of three years.
Dental composite materials are tooth-colored and are exposed to components in the oral environment such as saliva and food. It is desired that the restorations maintain their color stability under these conditions.24 In the in vitro study conducted by Hatırlı et al., color change was detected at varying rates in all restorative materials and it was found that the most affected restorations were those made with microhybrid composites.25 Similarly, in our study, we observed that the restorations with higher Bravo scores that remained within clinically acceptable limits were in the microhybrid composite G-aenial Anterior, Aelite All Purpose Body and Nova Compo N groups.
In the study by Furness et al., marginal compatibility of bulk fill composites and conventional composites with enamel and dentin tissue showed similar results.26 In our study, we found that hybrid composites with fillers of different sizes maintained their anatomical form within clinically acceptable limits and gave Alpha and Bravo values for marginal adaptation and coloration.
Depending on the preference of the dentist, universal adhesives can be used in restoration construction in total etch, self-etch, and selective etch modes. Burke et al. did not etch in their study, considering the sensitivity that may occur in the dentin after etching, and recommended selective etching of the enamel if deemed necessary.27 In our study, restorations made with universal adhesives in self-etch mode were examined in order to prevent postoperative sensitivity. In restorations made in class II cavities including dentin tissue, no sensitivity was observed in any restoration after one year, while postoperative sensitivity was detected in only one restoration (G-aenial Anterior group) after three years.
In the study conducted by Josic et al. using universal adhesives; retention loss was found to be successful regardless of the application mode at 6 months follow-up, while statistical differences were shown at 12, 18 and 24 months follow-up. Higher retention loss was detected in the self-etch application mode compared to the total etch application mode group.28 In our study, while we did not observe any retention loss in the restorations after the application in self-etch mode at the end of one year, we noted retention loss in one restoration (Cleafil Photo Posterior group) after three years.
Conclusions
In our study where we evaluated the restorations retrospectively, we found that the dental composite materials used were clinically successful according to the Modified USPHS criteria, and when all criteria were evaluated, a total success rate of 98.6% was achieved. The life of the restorations depends on many factors such as the patient's oral hygiene, caries susceptibility, and the materials and techniques used. The patients evaluated in our study had good oral hygiene, no caries formationor periodontal problems, which explains the high success rates of the restorations. In line with the first aim of this study, as a result of the statistical evaluation of the data obtained from the Modified USPHS criteria, it was observed that there was a difference in Bravo scores between dental composite materials. Secondly,it was seen that the data obtained from all dental composite materials used in the study remained at the level of clinical acceptability and there was no clinical difference between the restorations.
Composite resins, which are in widespread clinical use,are successful and open to development. More studies monitoring the survivalrates of restorations in the mouth will guide understanding the nature of the material and making tooth-like restorations.
Acknowledgments
I would like to thank my professors at Selçuk University Faculty of Dentistry, Department of Restorative Dentistry, all my friends who helped me during the study, and my family who was always with me.
Conflicts of Interest
The authorsdeclare no conflictsof interes
References
-
Ei-Mowafy O, Lewis D, Benmergui C, et al. Meta-analysis on long-term clinical performance of posterior composite restorations. 1994; 22: 33-43.
View at Publisher | View at Google Scholar -
Ferracane JLJCRiOB and Medicine. Current trends in dental composites. 1995; 6: 302-318.
View at Publisher | View at Google Scholar -
Sherwood IA. Essentials of operative dentistry. Boydell & Brewer Ltd, 2010. Milnar FJC. The evolution of direct composites. 2011; 32: 2-3.
View at Publisher | View at Google Scholar -
Çelik ÇJTKJRD-ST. Güncel Kompozit Rezin Sistemler. 2017; 3: 128-137.
View at Publisher | View at Google Scholar -
Uluakay M, Hüseyin İ, Yamanel K, et al. Kompozit rezinler ve polimerizasyon büzülmesi. 2011; 5: 895-902.
View at Publisher | View at Google Scholar -
Sarrett DCJDm. Clinical challenges and the relevance of materials testing for posterior composite restorations. 2005;21: 9-20.
View at Publisher | View at Google Scholar -
Bayne SC, Heymann HO and Swift Jr EJJJotADA. Update on dental composite restorations. 1994; 125: 687-701.
View at Publisher | View at Google Scholar -
Altun CJGtd. Kompozit dolgu materyallerinde son gelişmeler. 2005; 47:77-82.
View at Publisher | View at Google Scholar -
Talib RJTJoNUSoD. Dental composites: a review. 1993; 35: 161-170.
View at Publisher | View at Google Scholar -
Roberson T, Heymann HO and Swift Jr EJ. Sturdevant's art and science of operative dentistry. Elsevier Health Sciences, 2006.
View at Publisher | View at Google Scholar -
Perez MM, Hita-Iglesias C, Ghinea R, et al. Optical properties of supra-nano spherical filled resin composites compared to nanofilled, nano-hybrid and micro-hybrid composites. 2016; 35: 353-359.
View at Publisher | View at Google Scholar -
Aw T and Nicholls JJOd. Polymerization shrinkage
View at Publisher | View at Google Scholar -
Hanks CT, Wataha JC and Sun ZJDM. In vitro models of biocompatibility: a review. 1996; 12: 186-193.
View at Publisher | View at Google Scholar -
Bal BT, Sönmez NA, Bavbek B, et al. Farklı kompozit
View at Publisher | View at Google Scholar -
Opdam N, Collares K, Hickel R, et al. Clinical studies in restorative dentistry: new directions and new demands. 2018; 34: 1-12.
View at Publisher | View at Google Scholar -
Bayne SC and Schmalz GJCoi. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. 2005; 9: 209-214.
View at Publisher | View at Google Scholar -
Ferracane JLJDm. Resin-based composite performance: are there some things we can’t predict? 2013; 29: 51-58.
View at Publisher | View at Google Scholar -
Ferracane JL, Lawson NCJJoE and Dentistry R. Probing the hierarchy of evidence to identify the best strategy for placing class II dental composite restorations using current materials. 2021; 33: 39-50.
View at Publisher | View at Google Scholar -
Büyükdere AK and Sertgöz AJAÜDHFD. Sabit Protetik Restorasyonların İn Vivo Çalışmalar İle Değerlendirilmesi. 2016; 25.
View at Publisher | View at Google Scholar -
Şeker M, Tağtekin D, YANIKOĞLU F, et al. Posterior
View at Publisher | View at Google Scholar -
Sistemleri. 2021; 42: 131-140.
View at Publisher | View at Google Scholar -
Maktabi H, Balhaddad AA, Alkhubaizi Q, et al. Factors influencing success of radiant exposure in light-curing posterior dental composite in the clinical setting. 2018; 31: 320-328.
View at Publisher | View at Google Scholar -
Nedeljkovic I, Teughels W, De Munck J, et al. Is secondary caries with composites a material-based problem? 2015; 31: e247- e277.
View at Publisher | View at Google Scholar -
Bagheri R, Burrow M and Tyas MJJod. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. 2005; 33: 389-398.
View at Publisher | View at Google Scholar -
Hatırlı H, Kılıç E and Karaarslan EŞJAÜDHFD. Ağız Gargaralarının Farklı Kompozit Rezinlerin Renk Stabilitesine Etkisi. 2021; 31: 584-590.
View at Publisher | View at Google Scholar -
Furness A, Tadros MY, Looney SW, et al. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. 2014; 42: 439-449.
View at Publisher | View at Google Scholar -
Burke FT, Lawson A, Green DJ, et al. What's new in dentine bonding?: universal adhesives. 2017; 44: 328-340.
View at Publisher | View at Google Scholar -
Josic U, Maravic T, Mazzitelli C, et al. Is clinical behavior of composite restorations placed in non-carious cervical lesions influenced by the application mode of universal adhesives? A systematic review and meta-analysis. 2021; 37: e503-e5
View at Publisher | View at Google Scholar






