Case Report | DOI: https://doi.org/BRCA-CR-25-018
Apical Hypertrophic Cardiomyopathy of Left ventricle
Abstract
Apical hypertrophic cardiomyopathy (apical HCM) is a rare variant of hypertrophic cardiomyopathy with a prevalence of 1-2 % in Asian population and carries a benign prognosis both in Asian and Japanese. It is usually silent in early stages and manifest in adults with a suspicion of typical ECG changes of giant T wave inversion in left precordial leads. Transthoracic echocardiography is the mainstay of non-invasive diagnosis and provide a heterogeneous appearance of it’s morphological features with a spade shaped LV (left ventricular cavity). Background of this case study described the echocardiographic manifestations of apical HCM in a 54 –year old asymptomatic male.
Introduction:
Apical hypertrophic cardiomyopathy (apical HCM) is an atypical phenotype of non-obstructive HCM (hypertrophic cardiomyopathy) and it is more prevalent in Japanese people [1]. Usually it is considered as a benign condition and is detected incidentally by echocardiography
1.1 Review of literature
Apical HCM was first described in Japan. Sakamoto et al, first described the ECG pattern and echocardiographic findings of apical HCM in 1976 [2] in Japanese patients. But it was Yamaguchi that described the syndrome and its ventriculographic features in 1979 [3]. Kubo and colleagues [4] used echocardiography in a cohort of 264 patients to define the imaging characteristics and, Chen et al [5] utilized 2D echocardiography to further classify apical HCM and to assess the wall thickness. Kitaoka et al found the apical HCM in 15% of Japanese and 3% of American patients of HCM. According to Segen’s Medical dictionary, apical left ventricular hypertrophy constitute up to 25% of all HCM in Japan, but less than 5% [6] ( 8-10% [7].[8]) of non-Japanese population. It is rare in the West ( 1 to 11%) [9], but more common in oriental people and accounts for 13-41% of all variants of HCM among Asian individuals [10], 16% of the entire HCM population in Chinese [11] and in Taiwan, it is 25% of all HCM [12]. Sakamoto et al, noticed the benign prognosis of apical HCM in a study on 200 patients in Japan [13].
Published Indian studies are limited for comparison and so this case had been reported.
2. Case Report
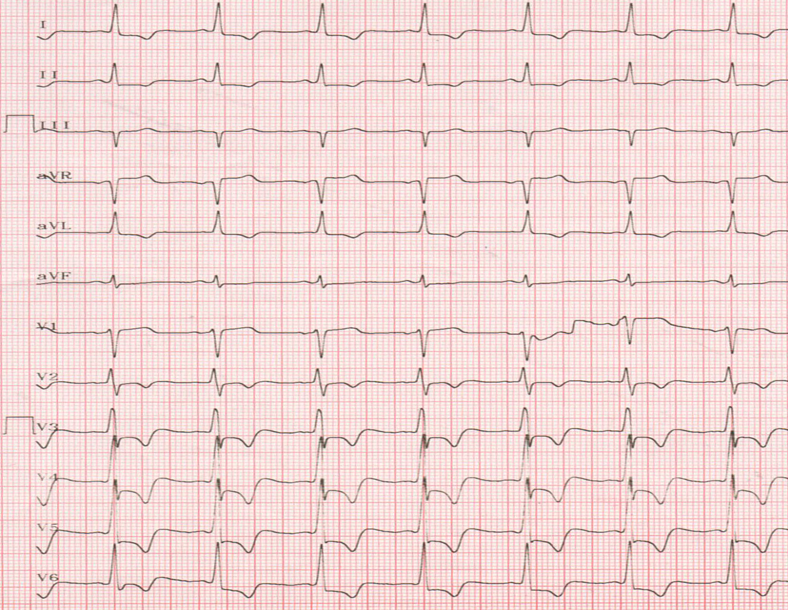
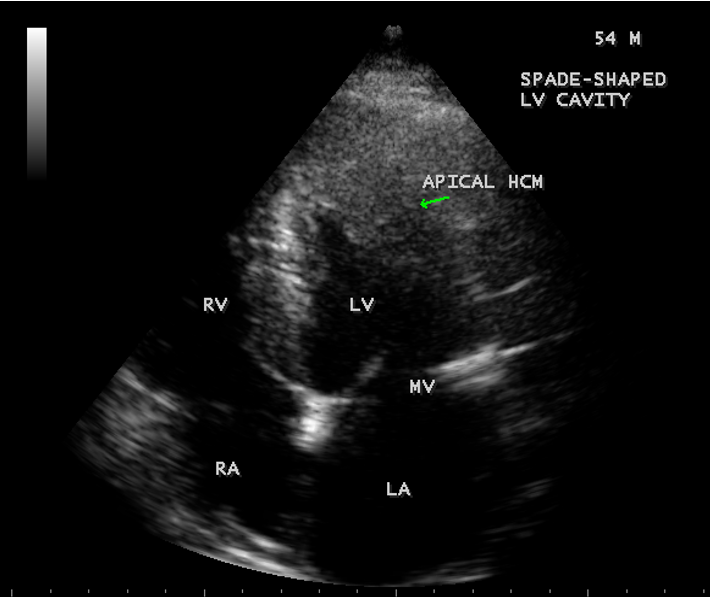
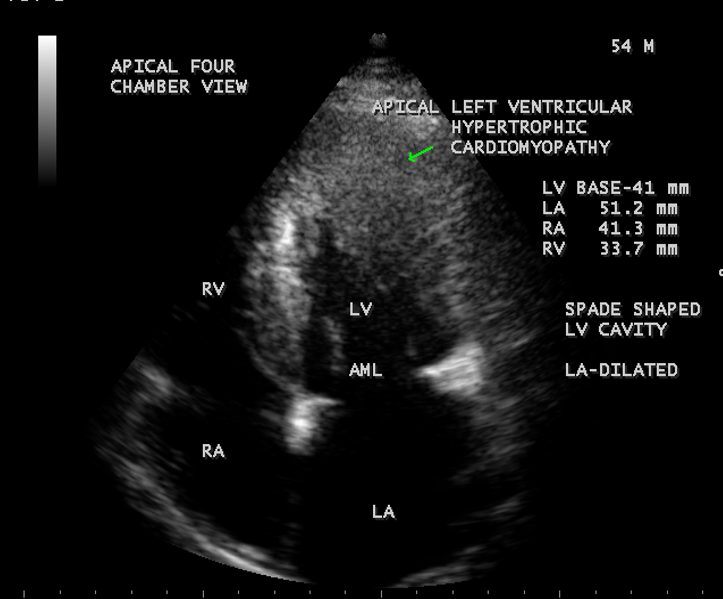
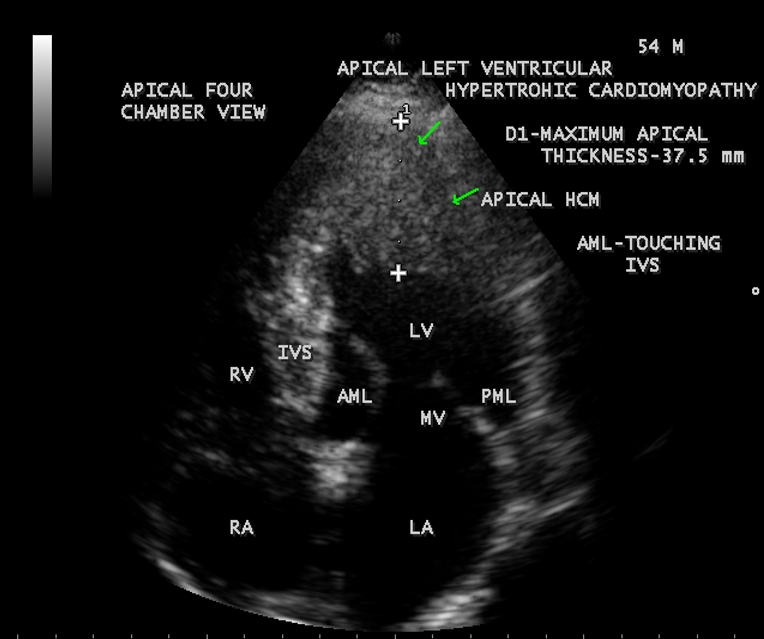
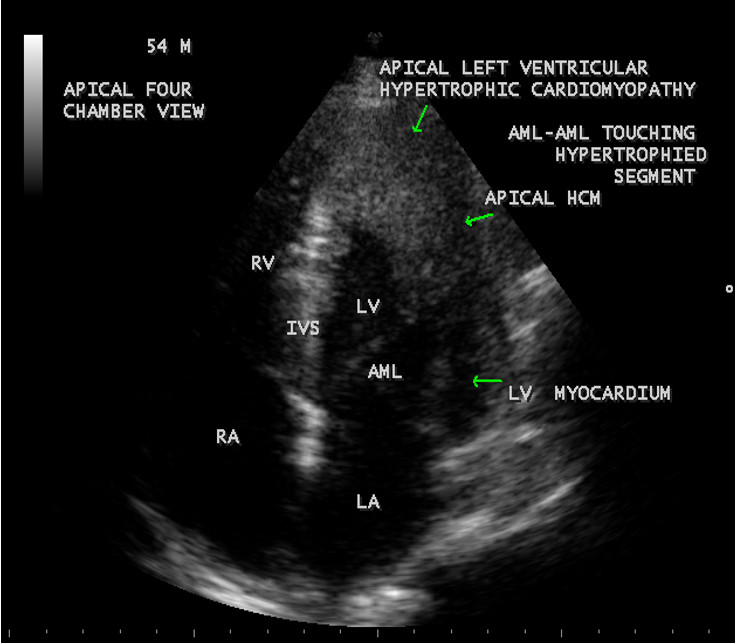
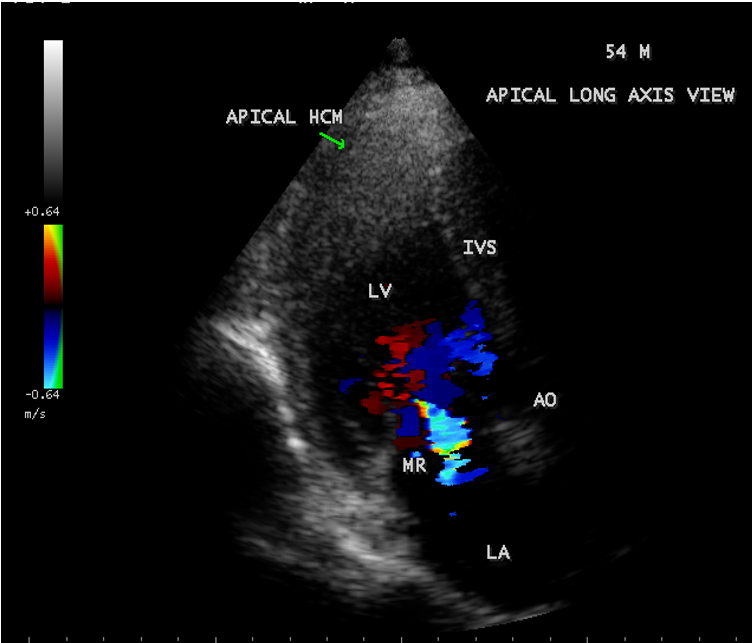
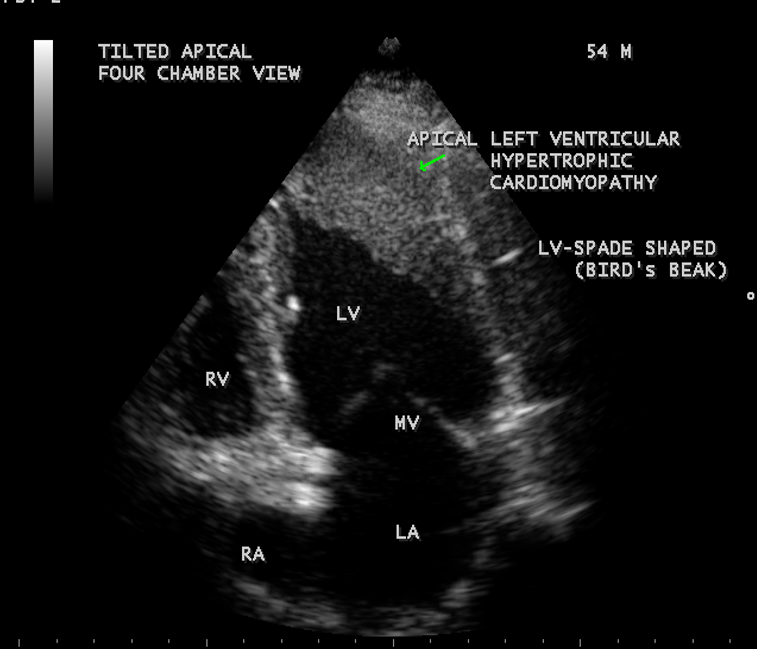
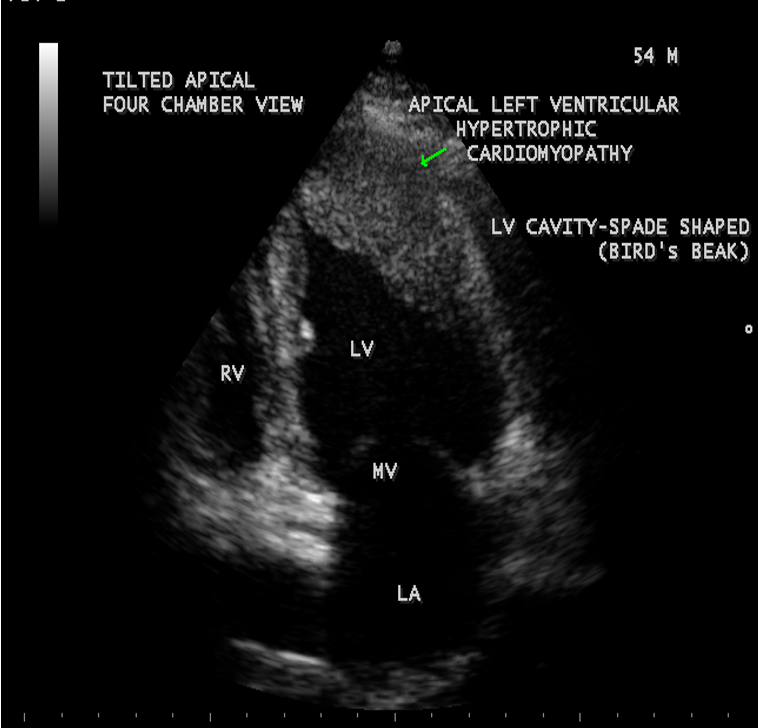
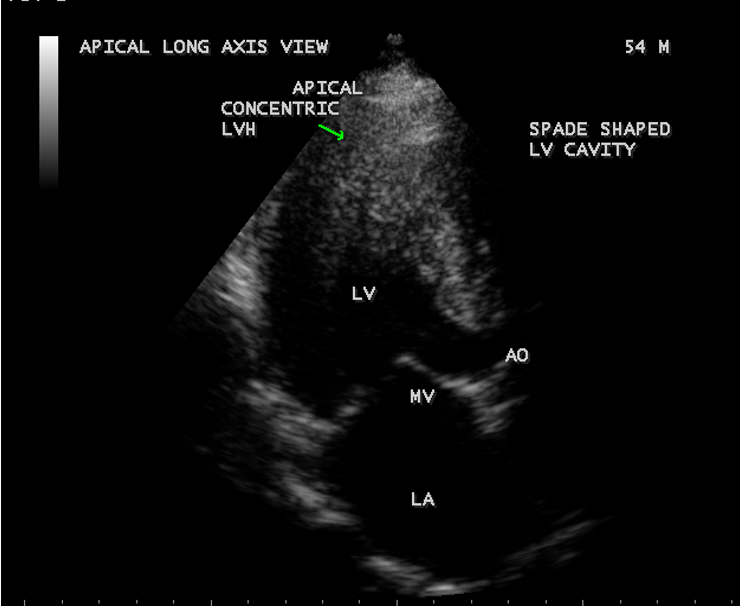
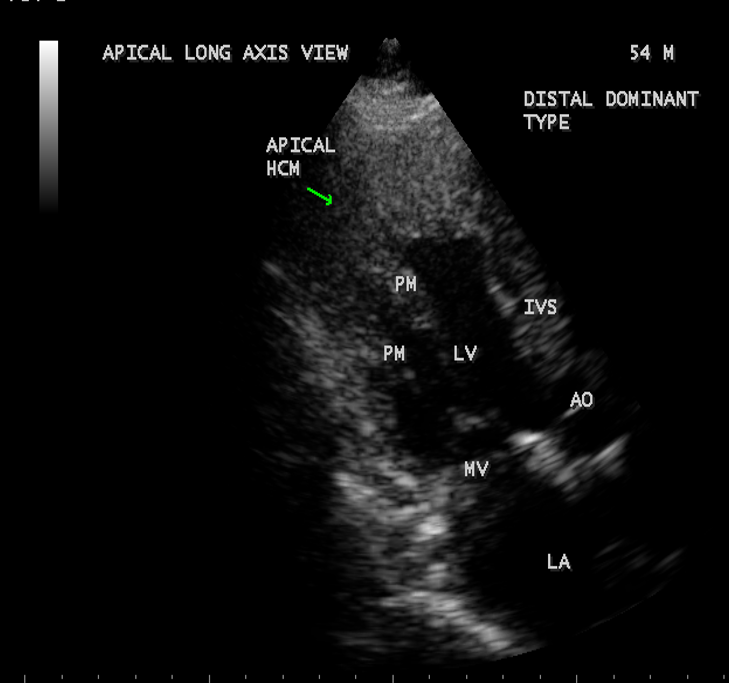
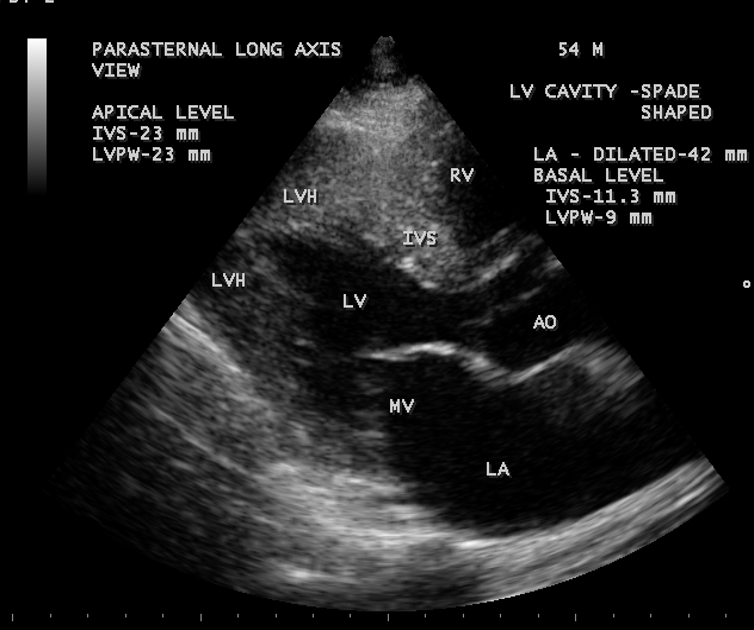
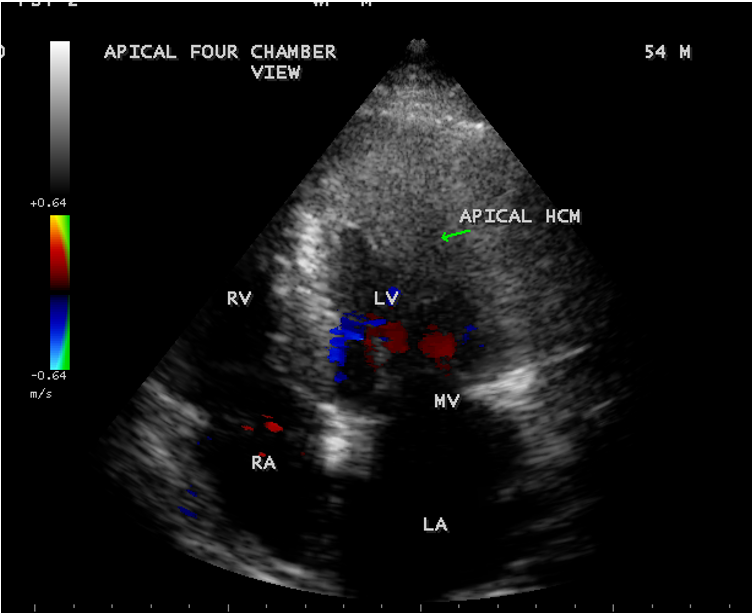
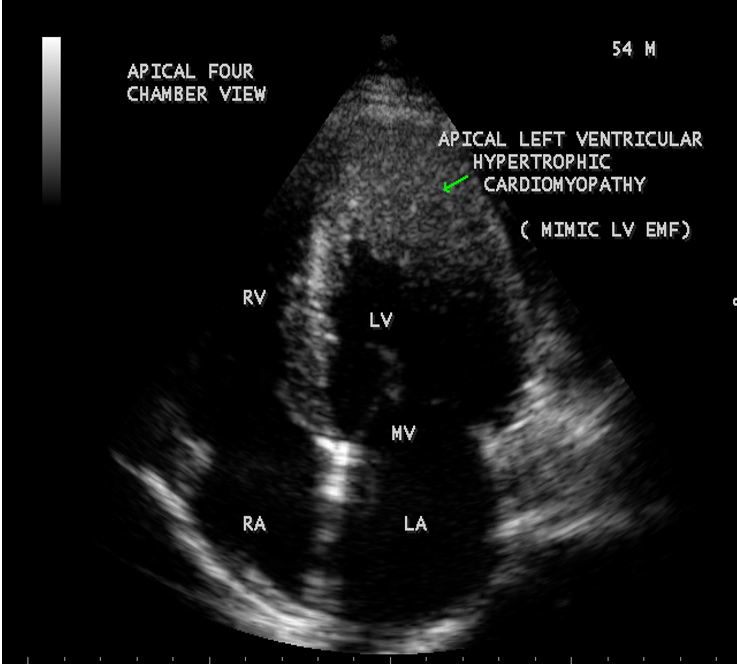
A 54-year-old asymptomatic male was referred for echocardiographic evaluation due to an LVH (left ventricular hypertrophy) pattern of ECG changes as shown in Figure A and a normal X-Ray chest. His pulse rate was 88 bpm and blood pressure 130/80 mmHg. Blood chemistry revealed normal. He had no physical findings. Transthoracic echocardiographic images revealed an asymmetric apical hypertrophy (AAH) in four chamber views and a concentric apical hypertrophic pattern in apical long axis view as shown in Figures given below. Screening of family members revealed normal and the patient was advised close follow up.
3.Discussion
3.1. Etiopathogenesis
Hypertrophic cardiomyopathy (HCM) is the most common genetically transmitted cardiovascular disease and it is usually familial with heterogeneous expression. Several disease-causing mutations in genes encoding proteins of the sarcomere have been reported [14]. A family history is more common in patients with asymmetric septal hypertrophy(ASH) than with apical hypertrophic cardiomyopathy (AHCM). Apical hypertrophic cardiomyopathy is frequently sporadic, a few families have been reported with autosomal dominant inheritance and a sarcomere gene mutation in the alpha-cardiac actin gene (Glu101Lys) has been shown to consistently producing the apical HCM phenotype [15]. Alpha and beta cardiac myosin heavy chain (MHC) mutations affect the polypeptides crucial to the structure of myofibrils and might be responsible for the myocyte and myofibrillar disarray, characteristic of familial HCM. The cause of sporadic apical HCM is unknown, but genetic, racial and even environmental factors could be responsible and many have lesser degree of hypertrophy, the outflow gradients are usually lacking, symptoms are often absent and the disease is detected only by echocardiography. An association with HLA-DR2 antigen in patients with apical HCM was recently reported in Japan [16]. Other investigators consider a secondary genesis as the underlying pathogenetic mechanism, ie, hypertension or heavy physical exercise [17].
Left ventricular hypertrophy is a gross anatomic marker and major determinant of the clinical feature of the disease [18]. The increased left ventricular mass is almost entirely due to increased wall thickness and the left ventricular cavity is usually small or normal in size. The distribution of wall thickening varies so greatly in HCM and there is no single classic morphologic pattern. Relatives with same genetic substrate usually have dissimilar pattern of left ventricular hypertrophy. All possible patterns of hypertrophy have been observed and occasionally, HCM shows segmental wall thickening confined to the left ventricular apex, a morphological form that in Japan has been associated with a spade shaped deformity of the left ventricle and giant negative T waves in electrocardiography (ECG)[19]. In some patients with HCM have substantial hypertrophy in unusual locations such as the posterior portion of the septum, the postero-basal free wall and the mid-ventricular level [20].
Embryologically, asymmetric septal hypertrophy results from postnatal persistence of a normal anatomic feature of the developing heart [21],[22]. The disproportionate thickening of the ventricular septum is characteristic of the normal embryonic and fetal human heart. Even though prominent hypertrophy may be found in infants, the typical patient develops left ventricular hypertrophy during adolescence [23] after a period of prolonged latency. However, HCM may occur at any time in adult life due to mutation of cardiac myosin-binding protein C [24].
3.2. Morphological types of apical HCM
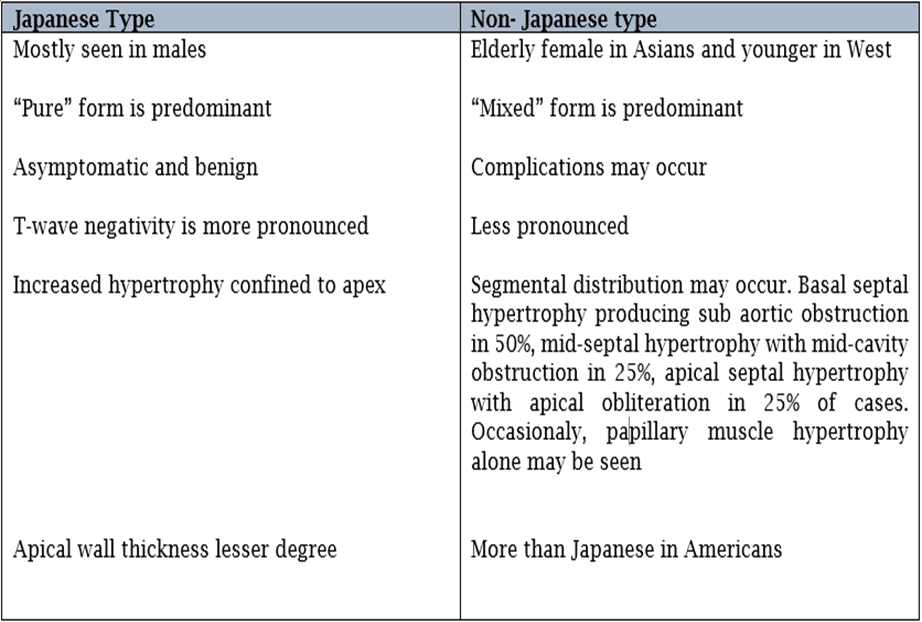
According to the distribution of hypertrophied musculature, the morphologic sub classification as “true apical” phenotype (hypertrophy of only the apical segment below the papillary muscle) and “ distal-dominant” phenotype (hypertrophy extended into the middle LV segments) have been recently recognized in North America [25]. Mid ventricular obstruction or apical obliteration was frequently found in patients with distal-dominant form and it is more often symptomatic and more likely to develop cardiovascular events. Other investigators have separated the AHCM into “pure form” (apical segment only) and “mixed form”(hypertrophy extending into other segments) [26]. Based on CMR (cardiac magnetic resonance) imaging, apical HCM is divided into 3 types as true apical form, a type with additional asymmetric involvement of ventricular wall segments and a type with symmetric involvement of ventricular wall segments. Generally, apical HCM is divided into two groups as isolated asymetric apical HCM (pure AHCM) and co-existent hypertrophy of interventricular septum (mixed AHCM)[27]. The pure form is predominant in Japanese, while the mixed form has been linked to Caucasian patients [28],[29].
3.3. Clinical Presentation
Clinical expression of apical HCM is highly variable. Apical HCM may manifest early in adulthood [30] and most series reported a mean age of atleast 41 years [31]. About 54 % of patients with apical HCM are symptomatic and the most common symptoms are chest pain, followed by palpitations, dyspnea and syncope. According to one large published series, AHCM presented with atypical chest pain (14%), palpitations (10%), dyspnea (6%), presyncope/syncope (6%)[32]. Atypical chest pain is the most frequent symptom and typical angina may also occur due to diminished vasodilaltory reserve. Atrial fibrillation (12%), apical myocardial infarction (10%), ventricular arrhythmia and apical thrombosis with subsequent embolization may occur up to 33% of cases [33]. [34]. The mismatch between fixed epicardial blood supply, and large muscle mass lead to sustained myocardial ischemia and necrosis resulting apical aneurysm which may complicate with ventricular tachycardia. A 65 – year old indian woman having apical aneurysm and presented with long standing angina had been reported [35].
3.4. ECG features
The most common ECG findings are negative T waves in the precordial leads, found in 93% of patients ( a depth > 10 mm in 47%) and a documented left ventricular hypertrophy on imaging is seen in 65% of patients with HCM. Giant T wave negativity (defined as depth or voltage >1 mV or 1.2 mV in any of the leads) in the left precordial leads is the hallmark feature of apical HCM and it may be due to balance of electrical forces emanating from the left versus the right ventricle [36] In 1983, Yamaguchi, et al published a report in 1979 determining that apical hypertrophy is the only specific hypertrophic pattern that shows characteristic ECG abnormalities, ie, giant negative T waves and high QRS voltage in the left precordial leads. Giant negative T waves are characteristic of hypertrophic cardiomyopathy with predominant apical thickening, especially in patients from the Pacific Rim, called as Yamaguchi syndrome [37].
Altered repolarization changes of ventricular myocardium may produce ST segment/ T wave changes in 70% of cases of left ventricular hypertrophy. There is significant variability on manifestation of strain pattern as minimally inverted or > 5 mm depth, asymmetric T wave with rapid return to baseline and terminal positivity, depression of the J point, T wave inversion in lead V6 > 3 mm and greater in V6 than V4 [38] and high QRS voltage (R in V5>26 mm, S in V1 + R in V5 ≥ 35 mm- positive Sokolo-Lyon index as a sign of LVH).
In apical HCM, larger degree of T wave inversions are seen and it’s depth does not correlate with severity of apical hypertrophy [39]. Presence of giant T wave inversions in Japanese HCM patients has been identified as a predictor of favourable outcome and it is more common in sporadic cases of apical HCM. Reports from outside Asia would suggest, however, that apical hypertrophy is uncommonly accompanied by marked T wave inversion and associated with adverse outcome in some patients. This heterogeneous morphologic expression even in first degree relatives is due to great dissimilarity in the pattern of left ventricular wall thickening [40]. In some non-Japanese studies, T wave negativity was often less pronounced and not necessarily localized to the precordial leads [41].
Abnormal ECG changes and no echocardiographic evidence of hypertrophic cadiomyopathy is seen in some patients due to abnormal gene in first degree relatives and called as carrier or preclinical state of hypertrophic cardiomyopathy. Incidence of deep T inversion may diminish considerably with advancing age. Myocardial infarction with a secondary apical LV aneurysm may occur in 10% of cases, that might determine the disappearance of the giant T waves in apical HCM and the “:spade” shaped LV configuration may become “ bottle-gourd “ shaped. In normal variant of hypertrophic cardiomyopathy (HCM), the LV (left ventricular) cavity is usually “banana” shaped. However, in some cases, non-giant T waves may become a giant one on later life. The T wave changes associated with ischemia are usually narrow and symmetric (deep T wave inversion) and “CVA (cerebrovascular accident)- T wave pattern” is associated with marked QT prolongation especially in subarachnoid hemorrhage.
3.5. Tranthoracic Echocardiography
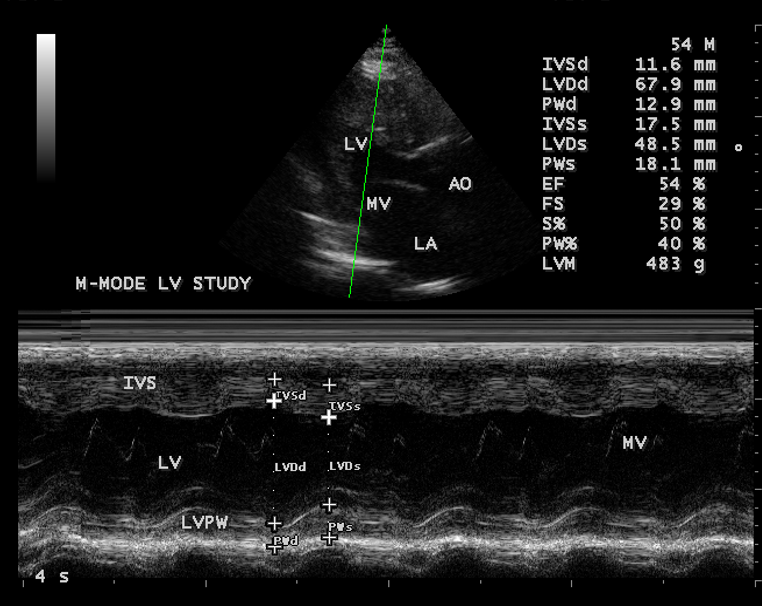
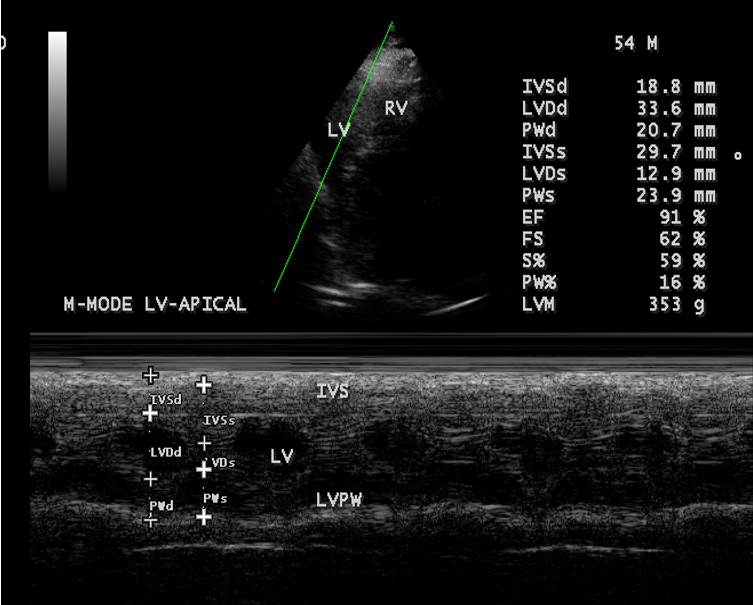
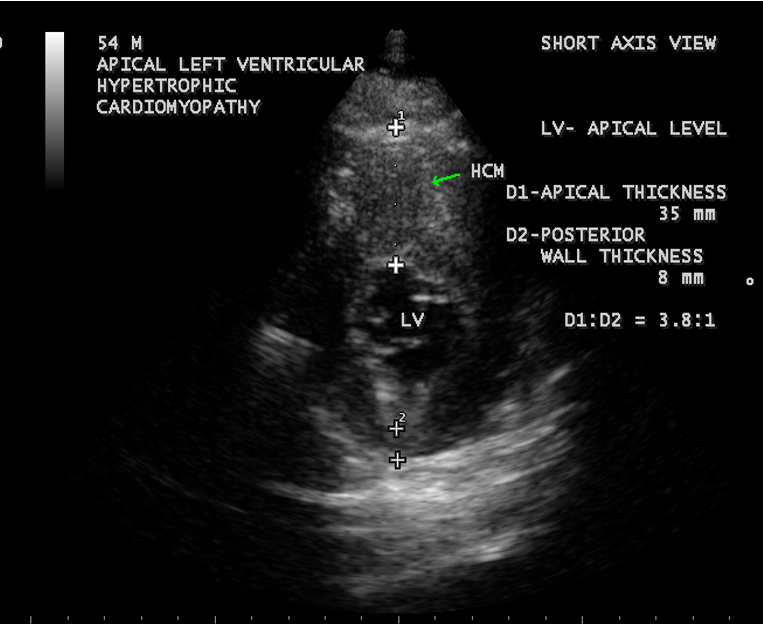
The preferred initial imaging test is Transthoracic Echocardiography and it is the most frequently utilized diagnostic modality [42]. Hypertrophy (apical or elsewhere) is defined as a compacted myocardial wall thickness in diastole greater than or equal to 14 mm and it is 15 mm as a threshold in conventional echocardiographic measurements, which was performed perpendicular to the axis of the wall and at the point of maximal thickness in short axis view at apical level as shown in Figure 14. In apical hypertrophic cardiomyopathy, the asymmetric hypertrophy of the left ventricle is predominantly confined to LV apex as shown in Figures 1 – 17, with a maximal apical thickness ≥ 15 mm and a ratio of maximal apical to posterior wall thickness ≥ 1.5 based on two dimensional echocardiography is a diagnostic criterion of apical HCM [43]. Figure 14 shows the maximal apical thickness of 35 mm and a ratio of maximal apical to posterior wall thickness(8mm) 4.4 : 1 ( > 1.3:1), satisfying the diagnosis of apical HCM in this patient.
Relative hypertrophy was defined as the absence of hypertrophy ( wall thickness < 14> 1). An apical- to-basal LV wall thickness ratio of 1.3-1.5 is diagnostic of apical HCM [44] and in this patient, it is 2 : 1 in parasternal long axis view as shown in Figure 10 and 1.6:1 as shown in Figures 12 and 13 in M-mode study at basal and apical levels and the range is 1.6-2:1 in this patient.
Apical HCM is characterized as concentric, circumferential hypertrophy of the entire apex due to apical left ventricular thickening of the anterior and posterior walls, resulting in a spade –like morphology of the left ventricular cavity during end diastole in LV long axis view of MRI and RAO projection of angiography. A subtype of apical HCM in which the distribution of hypertrophied myocardium proved to be confined to the apical lateral wall (AAH- asymmetric apical hypertrophy) and cannot be evaluated in long axis MRI or RAO projection in angiography and this subtype was called as non-spade apical HCM in short axis images of MRI [45]. A recent long-term study showed that patients with non-spade apical HCM may develop the typical spade-like configuration after some years [46]. Thus, the non-spade type is possibly an early stage of apical HCM and giant negative T waves are common in both types.
A criteria was formulated to diagnose apical HCM in a distinct phenotype not captured by existing disease classification. This phenotype comprises
Two essential criteria
- Deep ECG T wave inversion
- Relative apical hypertrophy (ABI > 1)
Four minor or supportive criteria
- Myocardial scarring by LGE CMR (late gadolinium enhancement cardiac magnetic resonance)
- Presence of apical aneurysm or microaneurysm
- Left atrial dilatation
- Apical cavity obliteration >20 mm
The presence of two or more of four minor criteria is the supportive evidence of apical HCM [47]. The differential features of Japanese and non-Japanese type of apical HCM is shown in the Table-1 given below.
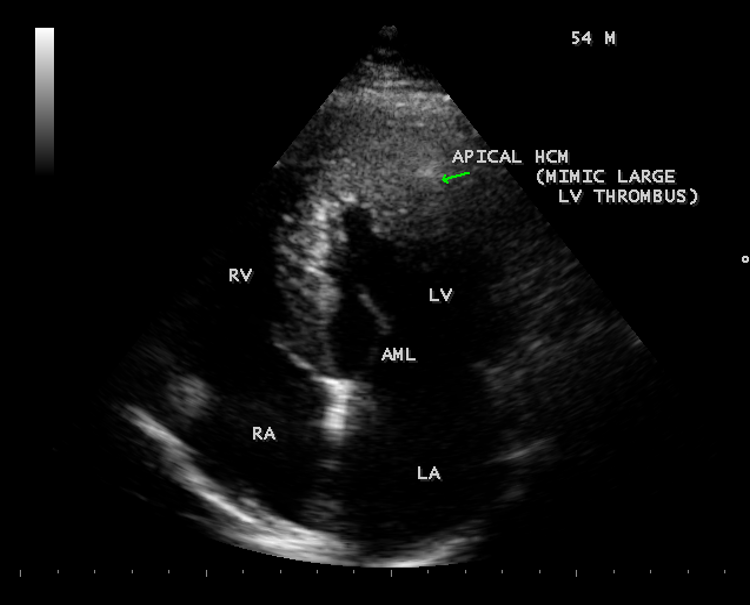
In transthoracic echocardiography, the lateral wall hypertrophy is more than the apical septum and producing a classical “ ace of spades sign” in apical four chamber [48] views as shown in Figures 1-4, 11 and 15 and tilted apical views as shown in Figures 6 and 7. In apical long axis view as shown in Figure 8 and parasternal long axis view as in Figure 10 , it is seen as concentric LVH pattern of apex with a spade shaped LV cavity and thus, resulting a heterogeneous appearance in echocardiographic images of various views. Interestingly, spade shaped configuration of LV cavity is visualized in all views in both systolic and diastolic images as assessed by the movement of mitral valve, Kitaoka et al, demonstrated that the wall thickness at the apex was greater in Americans (23 ± 4 mm) than in the Japanese patients(18 ± 2 mm). Duygu et al, shown that mean maximum apical thickness was 18 mm in a review of 17 patients with apical HCM. Figure 3 shows a maximum apical thickness 37.5 mm in apical 4 chamber view of this patient. The anterior mitral leaflet is long and elongated and mildly regurgitant as shown in Figure 5 due to trauma as a result of contact with septum and hypertrophied segment as shown in Figures 3 and 4.
Lateral wall thickening was smooth, homogeneous, non-trabeculated in apical HCM and thus differentiated from non-compacted LV (left ventricular) cardiomyopathy and apical HCM may mimic as apical LV thrombus as shown in Figure 15, but there is no wall motion abnormality was detected as shown in M-mode images of Figures 12 and 13 at basal and apical levels. It can also mimic LV EMF as shown in Figure 16, but EMF is characterized with firm, rolled edges and a rugose surface over the endocardium
3.6. Treatment
Apical HCM is generally associated with good prognosis in both Asian and Caucasian population and a long-term mortality is 0.1% per year. The approach to management of apical HCM depends on symptoms and risk of sudden cardiac death (SCD). There is lesser incidence of sudden cardiac death in apical variant, compared to patients with normal variant HCM.
In asymptomatic patients, no specific therapy has been outlined, but counseling is certainly recommended for symptomatic monitoring to notice any syncope or presyncopal events on follow up. The medical regimen in symptomatic patients primarily consists of beta-blockers, which have been shown to decrease symptoms as well as overall mortality [49].
The major clinical features associated with increased risk of SCD in HCM patients are non-sustained ventricular tachycardia, maximum LV wall thickness of ≥ 3 cm, family history of SCD at younger age, unexplained syncope, abnormal BP response during exercise and increased left atrial diameter as a potential SCD risk modifier. Current guidelines do not recommend ICD (implantable cardioverter defibrillator) implantation as a primary prevention for SCD in apical HCM and these clinical features should be used to assess the prognosis on follow up.
In apical HCM complicated with apical aneurysm formation, the size and symptoms of the aneurysm were ameliorated by sub selective coronary angiography and alcohol injection into the small vessels supplying a limited segment of mid-LV obstructive muscle. Others have reported the use of surgical apical myectomy in similar circumstances [50].
An increased apical thickness of 3.75 cm and LA dilatation predict this patient as a high-risk category and so close monitoring is recommended in cardiologic clinic.
4.Conclusion:
The initial echocardiographic evaluation was sufficient to diagnose the patients with apical HCM [51]. Typical ECG changes of LVH (left ventricular hypertrophy) with pronounced negative T waves ( ≥1mV) is an indication for echocardiographic evaluation as a non-invasive assessment to detect apical hypertrophy. Transthoracic echocardiographic findings may vary with the extension of hypertrophy and in apical HCM, the obliteration of apical cavity by the hypertrophy resulting in a spade-shaped LV (left ventricular cavity) in all views of echocardiographic imaging was recognized in this patient and it remains aymptomatic in this 54-year old male at this belt of Thoothukudi in India
References
-
Kitaoka, H., Doi, Y.,Casey, S.,A.,Hitomi,N., Furuno,T.,Maron, B.,J.,(2003) Comparison of Prevalence of Apical Hypertrophic Cardiomyopathy in Japan and the United States. American Journal of Cardiology, 92, 1183-1186
View at Publisher | View at Google Scholar -
Sakamoto, T.,Tei, C.,Murayama, M.,et al(1976) Giant T wave inversion as a Manifestation of Asymmetrical Apical Hypertrophy of the Left Ventricle: Echocardiographic and Ultrasono-Cardiotomographic Study. Japanese Heart Journal, 17, 611-629
View at Publisher | View at Google Scholar -
Yamaguchi,H., Ishimura,T.,Nishiyama, S., et al(1979) Hypertrophic Non-Obstructive Cardiomyopathy with Giant negative T waves (apical hypertrophy): Ventriculographic and Echocardiographic Features in 30 Patients. American Journal of Cardiology, 44(3), 401-412
View at Publisher | View at Google Scholar -
Kubo,T.,Kitaoka, H.,Okawa, M., et al (2009)Clinical Profile of Hypertrophic Cardiomyopathy with Apical Phenotype-Comparision of Pure- Apical Form and Distal- Dominant Form, Circulation Journal, 73(12), 2330-2336.
View at Publisher | View at Google Scholar -
Chen, C.,C.,Lei,M.,H.,Hsu,Y.,C., Cheng Sung, Y.,J., (2011) Apical Hypertrophic Cardiomyopathy Correlations Between Echocardiographic Parameters, Angiographic Left Ventricular Morphology, and Clinical Outcomes, Clinical Cardiology, 34(4), 233-238
View at Publisher | View at Google Scholar -
Farlex (2003-2015), Segen’s Medical Dictionary.
View at Publisher | View at Google Scholar -
Huda,Y., Sakamoto, T., Amano,K., Yamaguchi,T., Takenaka, K., Takahoshi,H.,et al(1987) Prevalence of Hypertrophic Cardiomyopathy in a Population of Adult Japanese Workers as Detected by Echocardiographic Screening, American Journal of Cardiology, 59, 183-184.
View at Publisher | View at Google Scholar -
Reddy,V.,Korcarz, C.,Weinert,L., Al-Sadir,J., Spencer,K.,C.,(1998) Circulation,98,235.
View at Publisher | View at Google Scholar -
Maron,B.,J.,(2002) Hypertrophic Cardiomyopathy, A Systematic Review, Journal of American College of Cardiology(JAMA), 287, 1308-1320.
View at Publisher | View at Google Scholar -
Chikamori,T., Doi, Y.,L.,Akizawa, M.,Yonezawa, Y.,Ozawa, T.,Mckenna,W.,J.,(1992)Comparison of Clinical, Morphological, and Prognostic Features in Hypertrophic Cardiomyopathy between Japanese and Western Patients, Clinical Cardiology, 15(11), 833-837.
View at Publisher | View at Google Scholar -
Yan,L.,Wang,Z.,Xu,Z.,Li,Y.,Tao,Y.,Fan, C.,(2012) Two Hundred and Eight Patients with Apical Hypertrophic Cardiomyopathy in China. Clinical Feature, Prognosis, and Comparison of Pure and Mixed Forms, Clinical Cardiology,35(2).101-106
View at Publisher | View at Google Scholar -
Lee, C.,H, Liu, P.,Y., Lin, L.,J, et al (2006) Clinical Features and Outcome of Patients with Apical Hypertrophic Cardiomyopathy in Taiwan,Cardiology, 106, 29-35.
View at Publisher | View at Google Scholar -
Sakamoto, T.,(2001) Apical Hypertrophic Cardiomyopathy, an Overview, Journal of Cardiology, 37, supplement 1, 161-178
View at Publisher | View at Google Scholar -
Marian,A.,J.,Roberts,B.,(1995) Recent Advances in the Molecular Genetics of Hypertrophic Cardiomyopathy, Circulation, 92, 1336-1347
View at Publisher | View at Google Scholar -
Arad,M., Penas-Lado,M.,Monserrat,L., Maron,B.,J., Sherrid,M., Ho, C.,Y.,Barr,S., Karim,A., Olson,T.,M.,Kamisago,M., (2005) Gene Mutations in Apical Hypertrophic Cardiomyopathy, Circulation,112,2805-2811.
View at Publisher | View at Google Scholar -
Kishimoto,C.,Takada,H.,Hiraoka,Y.,et al(1996) HLA-DR2 Antigen Linkage in Patient with Apical Hypertrophic Cardiomyopathy in Japan, Cardiology, 87, 488-491
View at Publisher | View at Google Scholar -
Webb, J.,G.,Sasson,Z., Rakowski,H., et al (1990)Apical Hypertrophic Cardiomyopathy, Clinical Follow Up and Diagnostic Correlates, Journal of American College of Cardiology, 1583-1590.
View at Publisher | View at Google Scholar -
Maron,B.,J.,Gross,B.,W.,Stark,S.,J.,(1995) Extreme Left Ventricular Hypertrophy, Circulation, 92,2748
View at Publisher | View at Google Scholar -
Alfonso, F., Nihoyannopoulos, P.,Stewart, J.,et al (1990)Clinical Significance of Giant Negative T Waves in Hypertrophic Cardiomyopathy. Journal of American College of Cardiology, 15,965-971
View at Publisher | View at Google Scholar -
Maron,B.,J.,(1993)Hypertrophic Cardiomyopathy. Current Problems in Cardiology, 18,639.
View at Publisher | View at Google Scholar -
Skinner,J.,R.,Manzoor,A., Heyes, A.,M.,et al (1997) A Regional Study of Presentation and Outcome of Hypertrophic Cardiomyopathy in Infants, Heart, 77, 229-233
View at Publisher | View at Google Scholar -
Maron,B.,J.,Verter,J.,Kapur,S.,(1978) Disproportionate Ventricular Septal Thickening in the Developing Normal Human Heart, Circulation, 57, 520-526
View at Publisher | View at Google Scholar -
Maron,B.,J (1997) Hypertrophic Cardiomyopathy, Lancet, 350,127
View at Publisher | View at Google Scholar -
Nimura,H.,Bachinski,l.,l.,Sangwatanaroj,S.,et al(1998),Mutation in the Gene for Cardiac Myosin –Binding Protein C and Late –Onset Familial Hypertrophic Cardiomyopathy. New England Journal of Medicine, 338, 1248.
View at Publisher | View at Google Scholar -
Gruner,C.,Care,H.,Siminovitch,K.,Moravsky,G.,Wigle,E.,D.,Woo,A.,Rakowski,H.,(2011) Sarcomere Protein Gene Mutations in Patients with Apical Hypertrophic Cardiomyopathy, Circulation Cardiovascular Genetics, 4(3),288-295
View at Publisher | View at Google Scholar -
Choi,E.,Y., Rim,S.,J., Ha,J.,W., Kim,Y.,J.,Lee,S.,C.,Hang,D.,H., et al(2008) Phenotypic Spectrum and Clinical Characteristics of Apical Hypertrophic Cardiomyopathy: Multicenter Echo-Doppler Study, Cardiology, 110(1),53-61
View at Publisher | View at Google Scholar -
Abinader,E.,G., Ranchfleisch,S., Naschitz,J.,(1982)Hypertrophic Apical Cardiomyopathy A subtype of Hypertrophic Cardiomyopathy. Israel Journal of Medical Sciences,18(1),1005-1009
View at Publisher | View at Google Scholar -
Matsumori,A., Ohashi,N.,Sasayama,S.,(1998) Hepatitis C virus Infection and Hypertrophic Cardiomyopathy. Annals of Internal Medicine,129, 749-750.
View at Publisher | View at Google Scholar -
Louie,E.,K.,Maron,B.,J.,(1987)Apical Hypertrophic Cardiomyopathy: Clinical and Two-Dimensional Echocardiographic Assessment. Annals of Internal Medicine, 106, 663-670.
View at Publisher | View at Google Scholar -
Maron,B.,J.,Spinto,P.,Wesley,Y.,Arce,J.,(1986)Development and Progression of Left Ventricular Hypertrophy in Children with Hypertrophic Cardiomyopathy. New England Journal of Medicine,315(10),610-614
View at Publisher | View at Google Scholar -
Klarich,K.,W.,AttenhoferJost, C.,H.,Binder,J., Connolly,H.,M., Scott,C.,G.,Freeman,W.,K., Ackerman,M.,J., et al(2013)Risk of Death in Long-Term Follow-up of Patients with Apical Hypertrophic Cardiomyopathy, American Journal of Cardiology, 111(12),1784-1791
View at Publisher | View at Google Scholar -
Eriksson,H.,J.,Sonnenberg,B.,Woo,A.,Rakowski,P.,Parker,T.,A.,Wigle,E.,D.,Rakowski,H.,(2002)Long-term Outcome in Patient with Apical Hypertrophic Cardiomyopathy, Journal of American College of Cardiology, 39,4, 638-645.
View at Publisher | View at Google Scholar -
Prasad,K.,Atherton,J.,Smith,G.,C.,Mckenna,W.,J.,Frenneaur,M.,P.,.Nihoyannopoulos,P.,(1999) Echocardiographic Pitfalls in the Diagnosis of Hypertrophic Cardiomyopathy, Heart, 82(Supplement 3),1108-1115.
View at Publisher | View at Google Scholar -
Duygu,H.,Zoghi,H.,Nalbiantgil,S.,Ozerkan,F.,Akilli,A.,Akin,M.,et al(2008) Apical Hypertrophic Cardiomyopathy Might Lead to Misdiagnosis of Ischemic Heart Disease, International Journal of Cardiovascular Imaging, Doi: 10.1007/S 10554-008-9317-7.
View at Publisher | View at Google Scholar -
Kulkreti,B.,B.,Ramakrishnan,S.,Gulati,G.,S.,Bhargava,R.,Seth,S.,(2012) Calcified Aneurysm of Left Ventricular Apex in Apical Cardiomyopathy, Texas Heart Institute Journal, 39(5), 758-760.
View at Publisher | View at Google Scholar -
Wigle,E.,D.Rakowski,H.,Kimball,B.,P., et al(1995)Hypertrophic Cardiomyopathy, Clinical Spectrum and Treatment. Circulation,92, 1680.
View at Publisher | View at Google Scholar -
Usui,M.,Inoue Suzuki,J.,et al(1993) Relationship Between Distribution of Hypertrophic and Electrocarsiographic Changes in Hypertrophic Cardiomyopathy. American Heart Journal, 126, 177-183.
View at Publisher | View at Google Scholar -
Hayden,G.,E.,Brady,W.,J.,Perron,A.,D.,Somers,M.,P.,Mattu,A.,(2002) Electrocardiographic T- Wave Inversion: Differential Diagnosis in the Chest Pain Patient.American Journal of Emergency Medicine,20(3),252-262
View at Publisher | View at Google Scholar -
Nishiyama,S.,Shiratori,K.,Nishimura,S.,Araki,R.,Takeda,K.,et al(1984)Correlation Between Left Ventricular Wall Thickness and the Depth of negative T wave in Apical Hypertrophic Cardiomyopathy. Journal of Cardiology, 14,281-288
View at Publisher | View at Google Scholar -
Ciro,E.,Nichols,P.,F.,Maron,B.,J.,(1983)Heterogeneous Morphologic Expression of Genetically Transmitted Hypertrophic Cardiomyopathy, Two-Dimensional Echocardiography, Circulation, 67,1227-1233.
View at Publisher | View at Google Scholar -
Maron,B.,J.,Bonow,R.,O.,Seshagiri,TNR, et al(1982)Hypertrophic Cardiomyopathy with Ventricular Septal Hypertrophy Localized to the Apical Region of the Left Ventricle (Apical Hypertrophic Cardiomyopathy), American Journal of Cardiology,49,1838-1848
View at Publisher | View at Google Scholar -
Stainback,R.,F.,(2012) Apical Hypertrophic Cardiomyopathy, Texas Heart Institute Journal, 39(5), 747-749.
View at Publisher | View at Google Scholar -
Camella,C.,Diaconu, Nicoleta Dumitru, Ana G. Fruntelata, Smarandita Lacau, Daniela Bartos (2015) Apical Hypertrophic Cardiomyopathy, The Ace- of- Spades as the Disease Card,Acta Cardiologica Sinica, 31(1), 83-86
View at Publisher | View at Google Scholar -
Chun,E.,J.,et al (2010)Hypertrophic Cardiomyopathy. Assessment with MR imaging and Multi-detected CT, Radiographics, 30,1309-1328
View at Publisher | View at Google Scholar -
Suzuki,J.,Watanake,F.,Takenaka,K.,et al (1993) New Type of Apical Hypertrophic Cardiomyopathy Identified with Nuclear Magnetic Resonance Imaging as an Underlyiong Cause of Markedly Inverted T Waves. Journal of American College of Cardiology,22,1175-1181.
View at Publisher | View at Google Scholar -
Suzuki,J.,Shimamoto,R.,Nishikawa,J.,et al(1999) Morphological Onset and Early Diagnosis in Apical Hypertrophic Cardiomyopathy. A Long-Term Analysis with Nuclear Magnetic Resonance Imaging,. Journal of American College of Cardiology,33, 146-151.
View at Publisher | View at Google Scholar -
Andrew S. Flett, Viviana Maestrini, Don Milliken, Mariana Fontana, Thomas A.Treibel, Rami Harb, Daniel M. Sado, Giovanni Quarta, Anna Herrey, James Sneddon, Perry Elliot, William McKenna, James C.Moon (2015), Diagnosis of Apical Hypertrophic Cardiomyopathy: T-Wave Inversion and Relative But Not Absolute Apical Left Ventricular Hypertrophy, International Journal of Cardiology, 183, 143-148
View at Publisher | View at Google Scholar -
Hemant Chaturvedi (2015) Apical Hypertrophic Cardiomyopathy with Hemodynamically Unstable Ventricular Arrhythmias. Atypical Presentation, EC (E- CRONICON) Cardiology, 22,106-110.
View at Publisher | View at Google Scholar -
Kim,S.,H., Kim,S.,O.,Han,S., Hwang,K.,W.,Lee,C.,W.,Nam,G.,R.,et al(2013) Long-Term Comparison of Apical versus Asymmetric Hypertrophic Cardiomyopathy, International Heart Journal, 54, 207-211.
View at Publisher | View at Google Scholar -
Schaff,H.,V.,Brown,M.,I.,Dearani,J.,A.,Abel,MD.,Ommen,S.,R.,Sorajja,P.,et al(2010) Apical Myectomy: A New Surgical Technique for Management of Severely Symptomatic Patients with Apical Hypertrophic Cardiomyopathy, Journal of Thoracic Cardiovascular Surgery,139(3), 634-640.
View at Publisher | View at Google Scholar -
Rodgers-Fischl,P.,Kolodziej,A.,R.,Sorrell,V.,I.,Rugg,S.,S.,(2016) Apical Hypertrophic Cardiomyopathy in an African American. A Case Presentation and Literature Review, Journal of Cardiology& Clinical Research,4(2), 1056
View at Publisher | View at Google Scholar






