Review Article | DOI: https://doi.org/BRCA-25-RW-019
A Review on Study of Asthma Symptom by Using Spirometry Test
Abstract
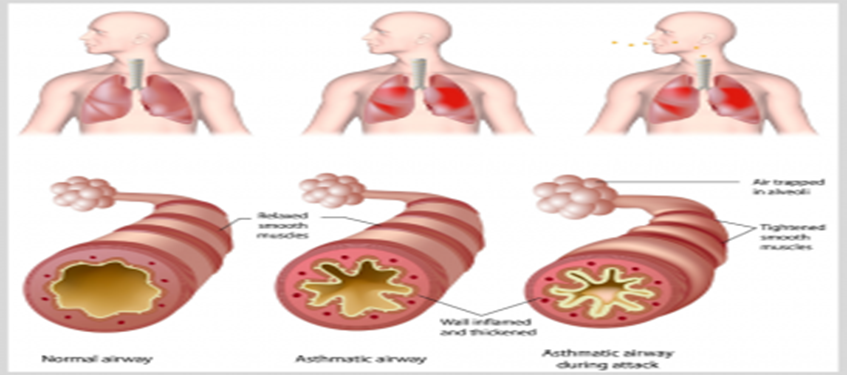
Asthma may be a common chronic disease with underlying inflammation of the airway. Advances in science have led to increased understanding of the heterogeneous nature of asthma and its complex mechanisms. Traditionally, asthma-practice guidelines have focused on optimizing lung function and therefore the US FDA has required increases in lung function and reduction of exacerbation as primary outcomes in clinical trials of new asthma therapeutics. Improved lung function may be a critical indicator of bronchodilator therapy, but the importance of long-term asthma control while maintained on controller medication is increasingly emphasized. The NIH asthma guidelines suggest the use of patient-reported outcomes, including health-related quality-of-life measures, to assess asthma control. Clinical practices and research studies concerning asthma can enjoy harmonizing the main outcome measures in order that comparisons across studies are often made. In this article, we review common asthma outcome measures with attention on recent efforts to harmonize outcomes for therapeutic clinical trials in asthma. The spirometry test may be a simple diagnostic assay administered employing a spirometer. A person will breathe into the tube attached to the spirometer, which records the results
Introduction
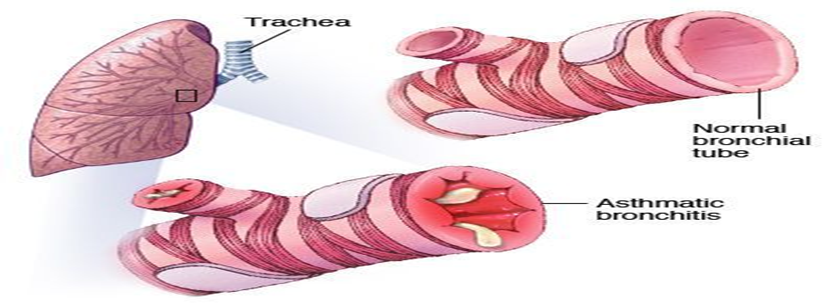
Asthma condition during which your airways narrow and swell and produce extra mucus. This will make breathing difficult and trigger coughing, wheezing and shortness of breath.
Asthma attacks are often mild, moderate, serious.Asthma cannot be cured, but its symptoms are often controlled. Because asthma often changes over time, it is vital that you simply work together with your doctor to trace your signs and symptoms and adjust treatment as required [1][2].
Symptoms
Asthma symptoms vary from person to person. you'll have infrequent asthma attacks, have symptoms only at certain times like when exercising or have symptoms all the time.[4]
- cough at night, when laughing, or during exercise
- whistling sound made when breathing
- Tightness in the chest During breathing
- Difficulty to breath
- Movement -induced asthma, which may be worse when the air is cold and dry
- Vocational asthma, triggered by workplace irritants such as chemical fumes, gases or dust
- Allergic-induced asthma, triggered by airborne substances, such as pollen, mold spores, cockroach waste or particles of skin and dried saliva shed by pets (pet dander)
- Heredity. Whether a parent has asthma, you’re more likely to develop it.
- History of viral infections. Patient with a history of viral infections during childhood are more likely to develop the condition.
- Early allergen exposure. Frequent contact with possible allergens and irritants may increase your risk for developing asthma.[1]
Risk factors
There are number of factors that increase your chances of developing asthma. These include:
- Possess a blood relative (such as a parent or sibling) with asthma
- Other allergic condition, such as atopic dermatitis or allergic rhinitis (hay fever)
- overweight
- a smoker
- Due to secondhand smoke
- Such exhaust fumes or other types of pollution
- occupational triggers, such as chemicals used in farming, hairdressing and manufacturing.[3]
Complications
- Asthma mainly consists of following complications
- Signs and symptoms that interfere with sleep, work or recreational activities
- Ill days from work or school during asthma flare-ups
- Lasting narrowing of the bronchial tubes (airway remodeling) that affects how well you can breathe
- Emergency room visits and hospitalizations for severe asthma attacks
- Side effects from long-term use of some medications used to stabilize severe asthma [3]
Spirometry:
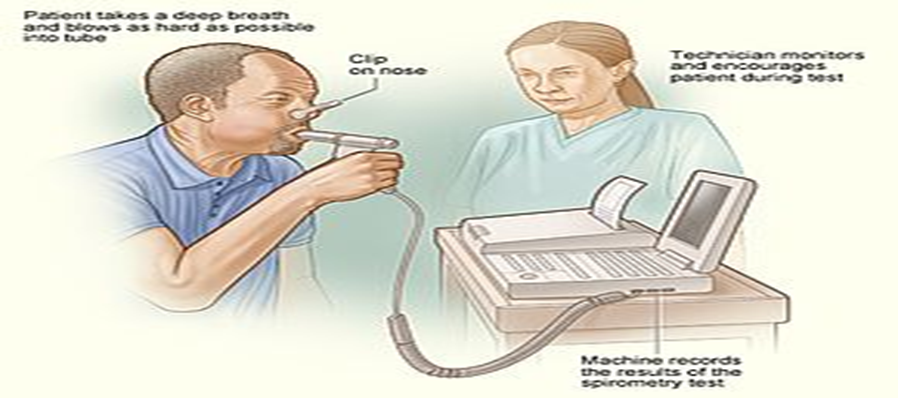
To take a spirometry test, you sit and breathe into a small machine called a spirometer. This medical device records the amount of air you breathe in and out and the speed of your breath.
Spirometry tests are used to diagnose these conditions:
- COPD
- asthma
- restrictive lung disease (such as interstitial pulmonary fibrosis)
- other disorders affecting lung function
They also allow your doctor to monitor chronic lung conditions to check that your current treatment is improving your breathing. Spirometry is often done as part of a group of tests known as pulmonary function.[3]
Procedure:
The spirometry test is a simple diagnostic test carried out using a spirometer. A person will breathe into the tube attached to the spirometer, which records the results.
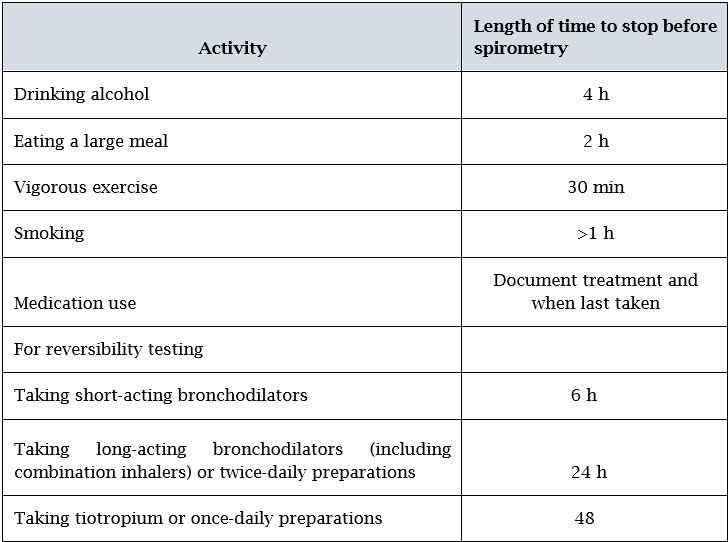
The doctor will ask a person about any breathing medications they may be taking, including bronchodilators. Bronchodilators help to relax the airways, widening them and making breathing easier. A person may be asked to stop taking these before the test so that their effect on breathing can be tested.
- Sit upright in a chair with your legs uncrossed and feet flat on the ground
- Breathe in completely and rapidly
- Pause for less than 1 second
- Place the spirometer mouthpiece in your mouth and close your lips to form a tight seal
- Breathe out as fast and as hard as possible, until your lungs are completely empty, or until you are unable to blow out any longer
- Breathe in completely and rapidly again
- Remove the mouthpiece
You will need to repeat the test at least three times to get the best result. Sometimes this may not be possible in one visit, because the test can be quite tiring.[4]
The test is not painful – it just needs you to put in your best effort to breathe out as hard as you can!
Sometimes you may be asked to do the spirometry test again after having some puffs of a ‘reliever’ medicine (usually a blue- or grey-colored puffer). The test will be done about 10 minutes after you’ve taken the reliever to check if the medicine helps your lungs to work better.
In adults, age, height, sex and race are the main determinants of the reference values for spirometric measurement.
- Age Lung function generally increases with age up to ∼25 years, then declines with increasing age afterwards. Unfortunately, some lung function equipment will give patients aged <25>
- Sex Pre-pubescent males and females generally have the same lung function, but post-puberty, the growth of the thorax is greater in males, giving marked differences in lung volumes
- Height The taller the person, the bigger the lungs.
- Weight Certain reference equations use weight to calculate reference values. Weight affects lung function in that increasing weight causes increasing lung function until obesity is reached, after which it has the opposite effect.
- Smoking This can cause a more rapid decline in lung function compared with nonsmokers over time. It should not be adjusted for in predicted equations, since any reduction is abnormal.[5]
FVC measurement:
One of the primary spirometry measurements is FVC, which is the greatest total amount of air you can forcefully breathe out after breathing in as deeply as possible. If your FVC is lower than normal, something is restricting your breathing.[3]
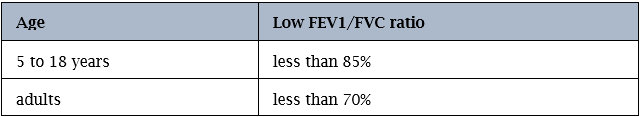
Normal or abnormal results are evaluated differently between adults and children:
For children ages 5 to 18:
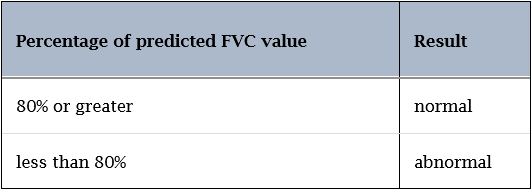
For adults:
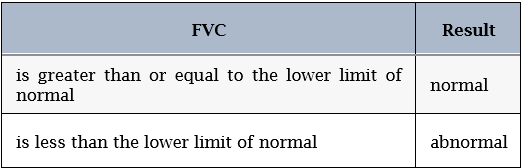
An abnormal FVC could be due to restrictive or obstructive lung disease, and other types of spirometry measurements are required to determine which type of lung disease is present. An obstructive or restrictive lung disease could be present by itself, but it’s possible to have a mixture of these two types at the same time
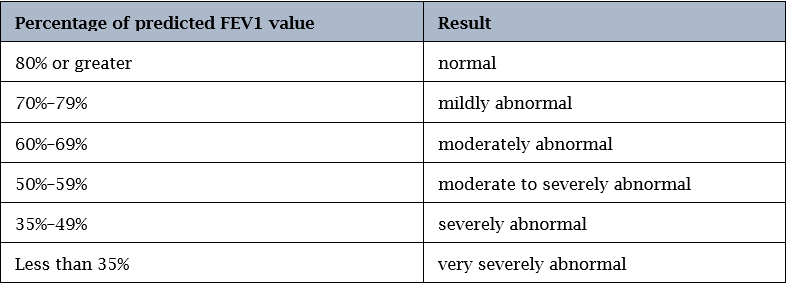
FEV1 measurement
The second key spirometry measurement is forced expiratory volume (FEV1). This is the amount of air you can force out of your lungs in one second. It can help your doctor evaluate the severity of your breathing problems. A lower-than-normal FEV1 reading shows you might have a significant breathing obstruction. [4]
Percentage of predicted FEV1 value
FEV1/FVC ratio
Doctors often analyze the FVC and FEV1 separately, and then calculate your FEV1/FVC ratio. The FEV1/FVC ratio is a number that represents the percentage of your lung capacity you’re able to exhale in one second. The higher the percentage derived from your FEV1/FVC ratio, in the absence of restrictive lung disease that causes a normal or elevated FEV1/FVC ratio, the healthier your lungs are. A low ratio suggests that something is blocking your airways
Spirometry Graph
Spirometry produces a graph that shows your flow of air over time. If your lungs are healthy and obstructive

Conclusion
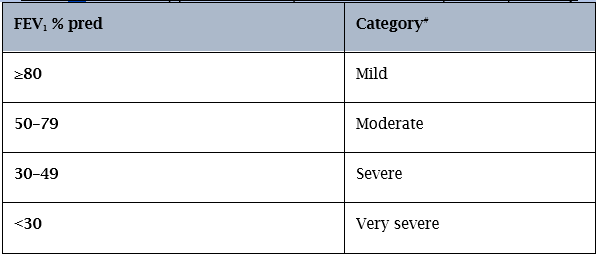
Asthma is an important chronic disease resulting in clinically significant morbidity, missed days of work or school, substantial costs for emergency care and hospitalization, and sometimes, death. Current therapy can control asthma and may prevent development of irreversible airway changes in asthmatic patients. Staging of COPD is driven by percent predicted FEV1 and FEV1/FVC ratio (providing the spirometry is carried out correctly); however, this takes only one piece of information into account. The authors advise that the reality of concordance of symptoms (according to the validated St Georges Respiratory Questionnaire38 and the newly developed short Clinical COPD Questionnaire)39 and the impact of COPD on a patient’s daily living according to their individual needs/occupation should be taken into account. Although it has been suggested that PEF can be used rather than spirometry,33 this is not the case in primary care, as the gold standard in diagnosing and tracking the path of COPD is spirometry, FEV1, and the FEV1/FVC ratio.
References
-
https://www.slideshare.net/HarithRiyadh/spirometry-functional-lung-test.
View at Publisher | View at Google Scholar -
https://www.mayoclinic.org/diseases-conditions/asthma
View at Publisher | View at Google Scholar -
https://asthma.ca/get-help/asthma-3/diagnosis
View at Publisher | View at Google Scholar -
Bronchial Asthma author M. Eric Gershwin Timothy E. Albertson
View at Publisher | View at Google Scholar -
The Pharmacy & Pharmacotherapy of Asthma Hardcover by James C. (editor) D'Arcy, Patrick F. (editor); McElnay (Author)
View at Publisher | View at Google Scholar -
https://www.healthline.com/health/spirometry#preparation
View at Publisher | View at Google Scholar






